Acute bronchitis
- Reviewed by Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
What is acute bronchitis?
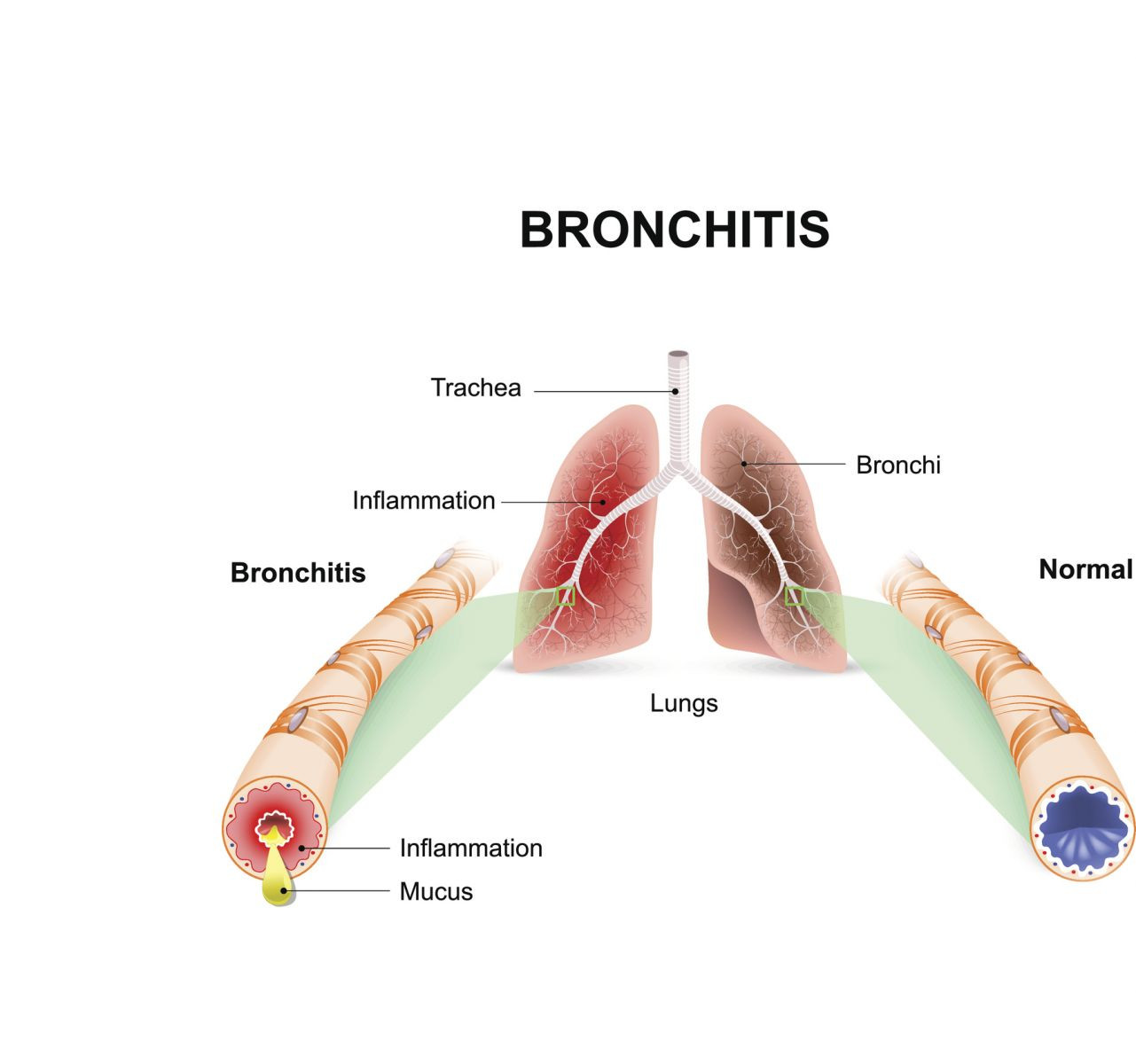
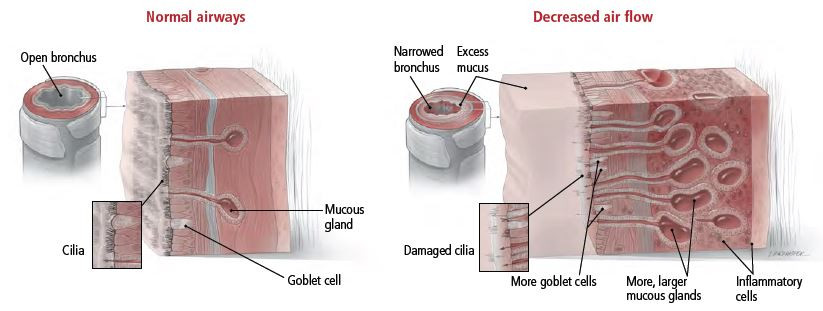
Acute bronchitis is an inflammation of the lining of the bronchial tubes, the hollow air passages that connect the lungs to the windpipe (trachea). The inflammation can be caused by an infection or by other factors that irritate the airways, such as cigarette smoking, allergies and exposure to fumes from some chemicals.
|
|
Acute bronchitis caused by an infection usually starts with an upper respiratory illness, such as the common cold or flu (influenza), that spreads from your nose and throat down into the airways. Acute bronchitis does not affect the lungs like pneumonia does. Pneumonia shows up on a chest X-ray, but acute bronchitis usually does not.
A respiratory virus causes about 90% of cases of acute bronchitis.
Symptoms of acute bronchitis
The main symptom of acute bronchitis is a cough. The cough can be dry or it can produce sputum, the mucus-like substance brought up from the lungs. The sputum may be clear, cloudy, brown, yellow or greenish. Other symptoms can include wheezing, chest tightness or pain, shortness of breath, sore throat, nasal congestion, fever and tiredness.
Diagnosing acute bronchitis
To diagnose acute bronchitis, your health care provider will ask about your medical history, especially whether you recently have had an upper respiratory infection. Your doctor also will listen to your chest with a stethoscope to try to detect sounds of wheezing and airways clogged with mucous. The level of oxygen in your blood may be tested using a small device that closes gently over a finger. If your health care provider hears any suspicious lung sounds during the physical examination, or if your oxygen level is lower than normal, he or she may order a chest X-ray to check for pneumonia.
Expected duration of acute bronchitis
Most cases of acute bronchitis go away without treatment within five days, although coughing usually lasts seven to 10 days. In some cases, coughing continues for weeks after the infection is gone because the bronchial linings are still irritated and may become narrow, as in asthma. Inhalers can help to treat the cough in these cases. When bronchitis comes back frequently or occurs most days of a month for at least three months of a year for two years, it is called chronic bronchitis. Chronic bronchitis occurs most often in current and former smokers.
Preventing acute bronchitis
There is no way to prevent all cases of acute bronchitis. However, the risk of bronchitis and complications can be reduced by not smoking and by getting flu, RSV and COVID vaccines to reduce the risk of getting one of these respiratory viruses, which can lead to acute bronchitis.
Treating acute bronchitis
Most cases of acute bronchitis do not require medical treatment. People diagnosed with acute bronchitis will be told to rest and drink plenty of fluids to keep the mucus thin, watery and easy to cough up. Warm, moist air also can loosen sputum and make coughing and breathing easier. Because of that, many physicians recommend at least one of the following for people with bronchitis:
- using a vaporizer or humidifier
- standing in or near a hot shower
- drinking hot tea or soup
- breathing in the steam from a sink or pot filled with hot water. You can catch more of the steam by tenting a towel over your head while bending over the water. For safety reasons, do not breathe from a pot of boiling water that is still on the stove.
If you have a fever, most physicians will recommend taking aspirin, ibuprofen (Advil, Motrin and others) or acetaminophen (Tylenol) to reduce fever. However, aspirin should not be given to children under age 19 to avoid the risk of Reye's syndrome, a rare but serious, potentially fatal illness that can occur when a child with a fever takes aspirin.
People who smoke should avoid smoking during the illness to reduce irritation to the airways.
If bronchitis is caused by a bacterial infection and doesn't get better on its own, an antibiotic may be prescribed. Antibiotics will be given only when there is a strong suspicion that the bronchitis is caused by a bacterial infection. That's because of rising concerns about antibiotic resistance, in which bacteria evolve in ways that allow them to survive antibiotics. This problem is increasing and is caused, in part, by antibiotics being used incorrectly and when they are not needed.
In some cases, doctors may prescribe a bronchodilator, an inhaled medication that helps the airways to open. These are the same medications used by some people with asthma to ease breathing during an asthma attack.
When to call a professional
You should call your doctor if:
- your breathing becomes difficult or painful
- you notice new wheezing or have worsening asthma symptoms
- you have a high fever that does not come down after taking a fever-relieving medication, such as acetaminophen or aspirin
- if you have fever that lasts more than three days
- your cough is getting worse or is producing bloody sputum.
Any time you have chest pain, you should call your doctor for advice. Chest pain can come from the heart as well as the lungs.
People at high risk of complications from acute bronchitis — such as infants, the elderly or people with chronic lung or heart disease — should call a physician at the first signs of bronchitis.
Symptoms of acute bronchitis are often similar to symptoms of mild asthma. People who have frequent bouts of acute bronchitis should make an appointment with a physician to see if they might have undiagnosed asthma or chronic bronchitis.
Prognosis
In an average, healthy person, acute bronchitis typically clears up quickly on its own or with antibiotic treatment. Some people, including the elderly, infants, smokers or people with heart or lung disorders, are at higher risk of developing complications from acute bronchitis.
Additional info
National Heart, Lung, and Blood Institute (NHLBI)
https://www.nhlbi.nih.gov
American Lung Association
https://www.lung.org
About the Reviewer

Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.