Crohn's disease
- Reviewed by Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
What is Crohn's disease?
Crohn's disease is an inflammatory bowel disease in which inflammation injures the intestines. It is a long-term (chronic) condition. Crohn's disease typically begins between ages 15 and 40.
No one knows for sure what triggers the initial intestinal inflammation at the start of Crohn's disease. A viral or bacterial infection may start the process by activating the immune system in the intestine. However, the immune system attack is not turned off: it stays active and creates inflammation even after the infection goes away.
Certain genes passed on from parent to child increase the risk of developing Crohn's disease, if the right trigger occurs.
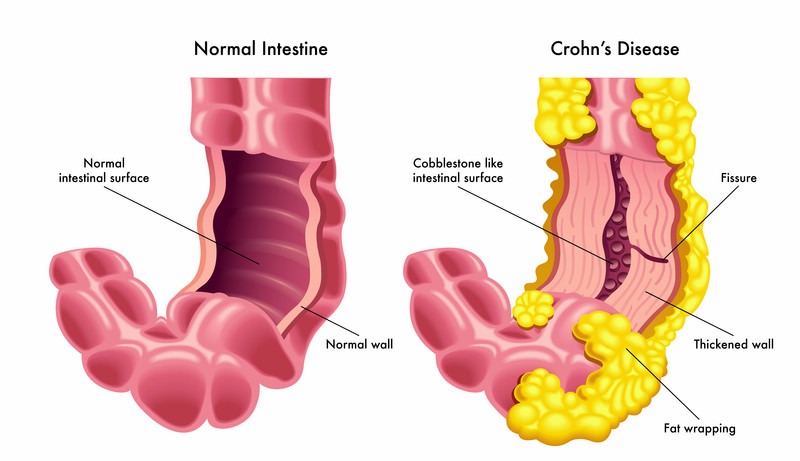
Once Crohn's disease begins, it can cause lifelong symptoms that come and go. The inner lining of the intestine thickens, and can wear away. The deeper layers of the intestine also become inflamed. This creates ulcers, cracks and fissures. Inflammation can allow an abscess (a pocket of pus) to develop.
A common complication of Crohn's disease is called a fistula. A fistula is an abnormal connection between two areas of the body; in Crohn's disease, the most common type is between two parts of the digestive tract, usually between one part of the intestine and another. A fistula can be created after inflammation becomes severe.
The section of the small intestine called the ileum is especially prone to damage from Crohn's disease. The ileum is located in the right lower abdomen. However, ulcers and inflammation can occur in all areas of the digestive tract, from the mouth to the rectum.
A few other parts of the body, such as the eyes and joints, also can be affected by Crohn's disease.
|
|
Symptoms of Crohn's disease
Some people with Crohn's disease have only occasional cramps, or diarrhea. Their symptoms are so mild they do not seek medical attention.
However, most people with Crohn's disease have more bothersome symptoms. They may experience long stretches of time with no symptoms. But these are interrupted by flare-ups of symptoms.
When Crohn's disease first begins, or during a flare-up, you might experience:
- abdominal pain, usually at or below the navel (typically worse after meals)
- diarrhea that may contain blood
- sores around the anus
- drainage of pus or mucus from the anus or anal area
- pain when you have a bowel movement
- mouth sores
- loss of appetite
- joint pains or back pain
- pain or vision changes in one or both eyes
- weight loss despite eating a normal-calorie diet
- fever
- weakness or fatigue
- stunted growth and delayed puberty in children.
Diagnosing Crohn's disease
If you have Crohn's disease, your symptoms and the results of various tests will usually fit a pattern over time that is highly suggestive of the diagosis. Even so, it may require months for your doctor to diagnose Crohn's disease with certainty.
Your doctor will look for evidence of intestinal inflammation. He or she will try to distinguish it from other causes of intestinal problems such as infection or ulcerative colitis. Ulcerative colitis is another disease that, like Crohn's diseases, also causes intestinal inflammation.
Test abnormalities that are often, but not always, found in people with Crohn's disease include:
- Blood tests. These may show a high white blood cell count or other signs of inflammation. Crohn's disease can interfere with the absorption of vitamin B12, which can lead to anemia, a reduced number of red blood cells: anemia and low levels of vitamin B12 can show up on blood tests.
- Autoantibody tests. Blood tests may reveal abnormal antibodies in the blood of people with Crohn's disease. They may help distinguish between Crohn's disease and ulcerative colitis.
- Stool tests. Also called feces or bowel movement tests, these may be useful to rule out infection as a cause of symptoms.
- Upper gastrointestinal (GI) series. This test uses x-ray pictures after you drink a barium solution. As the barium trickles down, it traces the outline of your intestines on the X-ray. An upper GI series can reveal places in the small intestine that are narrowed. It also can highlight ulcers and fistulas. These abnormalities are found more often in Crohn's disease than in ulcerative colitis, or other conditions that cause symptoms similar to those of Crohn's disease.
- Flexible sigmoidoscopy or colonoscopy. These tests use a small tube with an attached camera and light. The tube is inserted into your rectum, allowing your doctor to view the insides of your large intestine and obtain a biopsy (sample) of the lining tissue (see below).
- MR enterography. This relatively new test provides pictures of the entire intestine without radiation. It uses magnetic resonance imaging to show areas of Crohn's disease involvement.
- Wireless capsule endoscopy. The test involves swallowing a pill-sized object that is a tiny little video camera. It sends pictures of your small intestine wirelessly. Unlike x-ray studies such as the upper GI series, no x-ray radiation is involved.
- Biopsy. During colonoscopy or sigmoidoscopy, your physician can remove a small sample of tissue from the lining of the intestine. The material is examined in a laboratory for signs of inflammation. A biopsy is the most definitive test to confirm Crohn's disease and to exclude other conditions.
Expected duration of Crohn's disease
Crohn's disease is a lifelong condition. But it is not continuously active.
Following a flare-up, symptoms can stay with you for weeks or months. Often these flare-ups are separated by months or years of good health without any symptoms.
Preventing Crohn's disease
There is no way to prevent Crohn's disease.
But you can keep the condition from taking a heavy toll on your body. Maintain a well-balanced, nutritious diet to store up vitamins and nutrients between episodes or flare-ups. By doing so, you can decrease complications from poor nutrition, such as weight loss or anemia.
Also, do not smoke. Along with many other harmful health effects, smoking is a risk factor for developing Crohn's disease and is also linked to complications such as fistulas.
Crohn's disease can increase your risk of getting colon cancer. Have your colon checked regularly for early cancerous or precancerous changes. Check with your doctor regarding which types of tests to have and how frequently to repeat them.
Treating Crohn's disease
Medications are very effective at improving the symptoms of Crohn's disease. Most of the drugs work by preventing inflammation in the intestines.
For mild disease, steroids and/or anti-inflammatory drugs called aminosalicylates (such as mesalamine or sulfasalazine) are usually tried first. Aminosalicylates are chemically related to aspirin. They suppress inflammation in the intestine. They are given either as pills by mouth or by rectum, as an enema. Certain antibiotics help by killing bacteria in irritated areas of the bowel if infection is suspected or confirmed.
Antidiarrheal medications such as loperamide (Imodium) may be helpful if you have diarrhea.
Other more powerful anti-inflammatory drugs, such as azathioprine or 6-mercaptopurine, may be helpful. But they can also suppress your immune system, increasing your risk of infections. For this reason, they are not often used on a long-term basis. Combinations of these and some of the newer medications described below are commonly recommended.
Among the newest drugs approved for treatment of Crohn's disease are tumor necrosis factor (TNF) inhibitors and other injectable treatments. TNF is a substance made by immune system cells that causes inflammation. TNF inhibitors have potentially very serious side effects. They are generally prescribed for moderate to severe Crohn's disease that is not responding to other therapies and may be taken in combination with other medications. Adalimumab (Humira), certolizumab pegol (Cimzia), and infliximab (Remicade) are TNF inhibitors that have been found to improve Crohn's disease. When TNF inhibitors are not effective, other injectable options include ustekinumab (Stelara), risankizumab (Skyrizi), and vedolizumab (Entyvio).
Surgery to remove a section of the bowel is another possible treatment. In general, surgery is recommended only if a person has
- bowel obstruction
- persistent symptoms despite medical therapy
- a non-healing fistula.
When to call a professional
New or changing symptoms often mean that additional treatment is needed. People who have Crohn's disease should be in frequent contact with a doctor.
One serious complication is bowel obstruction. This occurs when the intestine becomes so narrowed that the digestive contents cannot pass through. Bowel obstruction causes vomiting or severe abdominal pain. It requires emergency treatment.
Other symptoms that require a doctor's immediate attention are:
- fever, which could indicate infection
- heavy bleeding from the rectum
- black, paste-like stools, which could indicate bleeding higher up in the intestinal tract.
Prognosis
Crohn's disease can affect people very differently. Many people have only mild symptoms. They do not require continuous treatment with medication.
Others require multiple medications and develop complications. Crohn's disease improves with treatment. It is not usually a fatal illness. While it can be controlled in most cases, it cannot be cured.
Crohn's disease requires people to pay special attention to their health needs and to seek frequent medical care. But it does not prevent most people from having normal jobs and productive family lives.
It can be helpful for a newly diagnosed person to seek advice from a support group of other people with the disease.
Additional info
Crohn's and Colitis Foundation of America
http://www.ccfa.org/
National Institute of Diabetes and Digestive and Kidney Disorders
http://www.niddk.nih.gov/
About the Reviewer

Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.