Rheumatoid arthritis
- Reviewed by Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
What is it?
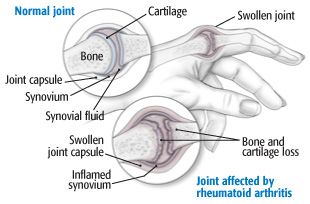
Rheumatoid arthritis is a chronic (long-lasting) inflammatory disease that causes pain, stiffness, warmth, redness and swelling in joints. Over time, the affected joints may become misshapen, misaligned and damaged. Tissue lining the joint can become thick, and may wear away surrounding ligaments, cartilage and bone as it spreads. Rheumatoid arthritis usually occurs in a symmetrical pattern, meaning that if one knee or hand has it, the other usually does, too.
|
|
The cause of rheumatoid arthritis is unknown, although it appears to be an autoimmune disease. When the body's immune system does not operate as it should, white blood cells that normally attack bacteria or viruses attack healthy tissue instead — in this case, the synovium, or joint tissue. As the synovial membrane (the thin layer of cells lining the joint) becomes inflamed, enzymes are released. Over time, these enzymes and certain immune cells damage the cartilage, bone, tendons and ligaments near the joint.
Some research suggests that a virus triggers this faulty immune response. However, there is not yet convincing evidence that a virus is the cause of rheumatoid arthritis. At the same time, it appears that some people are more likely to get the disease because of their genetics. Environmental factors may also be important. For example, smoking is a risk factor for rheumatoid arthritis.
Rheumatoid arthritis, the most disabling form of arthritis, generally affects more than one joint at a time. Commonly affected joints include those in the hands, wrists, feet, ankles, elbows, shoulders, hips, knees and neck. Rheumatoid arthritis can result in loose, deformed joints, loss of mobility and diminished strength. It also can cause painless lumps the size of a pea or acorn, called rheumatoid nodules. These develop under the skin, especially around the elbow or beneath the toes.
Generally, the pain of rheumatoid arthritis is described as a dull ache, similar to that of a headache or toothache. Pain is typically worse in the morning. It is not rare to have 30 minutes to an hour or more of morning stiffness. On days when the disease is more active, you may experience fatigue, loss of appetite, low-grade fever, sweats and difficulty sleeping.
Because rheumatoid arthritis is a systemic disease (meaning it can affect the entire body), you also may have inflammation in other areas, including the heart, lungs or eyes. Symptoms vary between people and even in one person over time. People with mild forms of the disease are bothered by pain and stiffness, but they may not experience any joint damage. For other people, damage occurs early, requiring aggressive medical and surgical treatment. People with rheumatoid arthritis may notice worsening and improvement for no apparent reason. Although this disease most often afflicts people between the ages of 20 and 50, it may affect children and the elderly. Of the 1.5 million people with rheumatoid arthritis in the United States, at least 75 percent are women.
Symptoms
Symptoms include:
- pain, swelling, limited motion, warmth and tightness around affected joints, which most commonly include the hands and wrists, feet and ankles, elbows, shoulders, neck, knees and hips, usually in a symmetrical pattern. Over time, joints may develop deformities.
- fatigue, soreness, stiffness and aching, particularly in the morning and afternoon (described as morning stiffness and afternoon fatigue)
- lumps or rheumatoid nodules below the skin
- weight loss
- low-grade fever and sweats
- trouble sleeping
- weakness and loss of mobility
- depression.
Other symptoms depend on whether other parts of the body are involved. For example, for those with lung involvement, shortness of breath is common.
Diagnosis
Your doctor will ask about your symptoms and medical history, and will examine you. You also may be sent for a blood test. An abnormal antibody, called the rheumatoid factor (RF), is found in the blood of 60 percent to 70 percent of patients with rheumatoid arthritis. However, having RF does not necessarily mean you have rheumatoid arthritis. Many people who do not have rheumatoid arthritis can have RF appear in their blood.
Another antibody, called the anti-cyclic citrullinated peptide (anti-CCP), is also present in about 65% of people with rheumatoid arthritis but it is a more specific indicator of rheumatoid arthritis — that is, few people without rheumatoid arthritis have this antibody. While it is more specific, the diagnosis of rheumatoid arthritis cannot be based solely on any single blood test. Other blood tests may be performed to look for other causes of joint pain.
While x-rays may be normal in the first few weeks or months of disease, joint damage (called erosions) may eventually appear. MRI or ultrasound may show evidence of joint inflammation earlier than x-rays.
You may hear about a checklist of symptoms (called criteria) for diagnosing rheumatoid arthritis. Although many physicians use this checklist as a guide, it is important to know that some patients with rheumatoid arthritis do not have many of the symptoms on the list, especially if their disease is mild. And some people with other forms of arthritis may meet criteria for rheumatoid arthritis.
The diagnosis of rheumatoid arthritis relies mostly on the experience and judgment of the doctor, and is based on the "big picture" of symptoms, examination and test results. The diagnosis also depends on excluding other explanations for the symptoms.
Expected duration
Most people with rheumatoid arthritis have chronic (long-lasting) symptoms. They experience periods when symptoms get worse, called flare-ups, and periods when symptoms improve. Rarely, symptoms and signs of the disease disappear without treatment, called a spontaneous remission.
Prevention
There is no way to prevent rheumatoid arthritis. However, smoking is a risk factor for rheumatoid arthritis. So this is one more reason not to smoke.
Treatment
The treatment of rheumatoid arthritis has improved dramatically in the past 50 years. A comprehensive approach that combines medications, rest balanced with exercise, lifestyle modifications, and sometimes surgery, can help many people to lead normal lives. The most important goals in treating rheumatoid arthritis are maintaining your ability to move and function, reducing pain, and preventing future joint damage. Early diagnosis and treatment are essential. If control of disease is achieved soon after symptoms begin, long-term outcomes tend to be good and quality of life and length of life may be normal. The treatments themselves may cause problems. You and your doctor will have to weigh the risks and benefits of any medication or other treatment that is available for this disease.
Medications
Certain medications relieve the symptoms of rheumatoid arthritis (such as pain and swelling), while other medications slow the progress of the disease.
Nonsteroidal anti-inflammatory drugs (NSAIDs), including over-the-counter aspirin, ibuprofen (Motrin and other brand names) and naproxen (Aleve, Naprosyn), or prescription NSAIDs can help relieve symptoms. Side effects occur in a minority of patients. These include upset stomach, ulcers, reduced kidney function or allergic reactions.
Newer NSAIDs, such as celecoxib (Celebrex), may provide the same benefits for arthritis as older medications but with less risk of ulcers. However, the risk of ulcers is not zero. One study showed that for people at highest risk (those with recent bleeding ulcer), up to 10 percent of those treated with celecoxib developed a new ulcer. In addition, the risk was similar for these high-risk patients taking celecoxib and those taking an older agent (diclofenac) combined with the acid blocker omeprazole. People taking celecoxib may also have a higher risk of cardiovascular problems (such as heart attack) than those taking other NSAIDs.
Other pain relievers, such as acetaminophen (Tylenol) or tramadol (Ultram), may provide pain relief when taken with or without an NSAID.
Corticosteroids, such as prednisone (Deltasone and other brand names), reduce inflammation. However, they have little lasting benefit and come with a long list of troubling side effects, such as easy bruising, thinning of the bones, cataracts, weight gain, puffy face, diabetes and high blood pressure, among others. If you do use corticosteroids, follow your doctor's recommendations closely. Your doctor may prescribe a corticosteroid to relieve occasional flare-ups, and then gradually taper you off the medication. Stopping corticosteroid therapy suddenly after taking it for more than a week or two can be dangerous.
Disease-modifying antirheumatic drugs (called DMARDs, second-line drugs or remittive therapy) appear to slow or halt the progression of rheumatoid arthritis by altering the function of your body's immune system. Most experts recommend that all people with rheumatoid arthritis take a DMARD soon after being diagnosed to reduce the chances of joint damage. These medications take weeks to months to start working. Therefore, your doctor probably may advise you to take an NSAID, a corticosteroid, or both during the early weeks or months of treatment with a DMARD.
These drugs include methotrexate (Folex, Methotrexate LPF, Rheumatrex), hydroxychloroquine (Plaquenil), leflunomide (Arava) or sulfasalazine (Azulfidine). Treatment commonly includes methotrexate as the initial choice but combinations of these medications (e.g., methotrexate, hydroxychloroquine and sulfasalazine) may be prescribed. Each of these comes with a risk of serious side effects. Your doctors will review them with you.
Newer medications, called "biologics" include:
- abatacept (Orencia)
- adalimumab (Humira)
- certolizumab (Cimzia)
- etanercept (Enbrel)
- golimumab (Simponi)
- infliximab (Remicade)
- rituximab (Rituxan)
- sarilumab (Kevzara)
- tocilizumab (Actemra)
These medications are available by injection only. They can be highly effective, but many patients improve with older medications that are much less expensive (and many health insurance companies will not cover biologics before older medications are tried first), so most doctors recommend older treatments first.
Newer medications, baricitinib (Olumiant), tofacitinib (Xeljanz), and upadacitinib (Rinvoq) are not biologic agents — they are called "Janus kinase (JAK) inhibitors" because they block an enzyme (Janus kinase) involved in inflammation. These medications offer patients another option for treatment, and while they are also quite expensive, they have one advantage over the other newer drugs: they are available in pill form.
Another drug for rheumatoid arthritis is anakinra (Kineret), an injectable drug that appears to be only modestly effective but may be a reasonable option if other treatments have failed. Other therapies include minocycline (Minocin), azathioprine (Imuran), cyclosporine (Neoral, Sandimmune), gold and penicillamine (Cuprimine, Depen). However, these treatments are used much less often now than in the past because most experts find that they are not as effective or safe.
Because the newest medications have generally been studied only in selected, and often the healthiest, people, they may have side effects that are not yet well known. For example, studies found that tuberculosis, although rare, was more common than expected among those receiving treatment with certain biologic agents. These findings have led to new recommendations about how patients should be screened before treatment begins.
Diet, exercise, and rehabilitation services
Finding a balance between rest and exercise is crucial to managing rheumatoid arthritis. When your symptoms flare up — when your joints are sore, warm and swollen — take it easy and rest. You can continue to do range-of-motion exercises to keep your joints mobile, but be careful not to tire yourself or aggravate your joints. Avoid unnecessary walking, housework or other activities. When your joints feel better and when other symptoms, including fatigue and morning stiffness, are less noticeable, increase your activity. Weight-bearing exercises such as walking and lifting weights can strengthen weakened muscles without risking additional joint damage. If exercise produces more pain or joint swelling, cut back a bit.
Despite many claims, there are no dietary changes, supplements, herbs, or other alternative therapies proven to control the symptoms of rheumatoid arthritis or protect the joints over a long period of time. However, a diet that helps you lose excess weight can be helpful for weight-bearing joints affected by rheumatoid arthritis. In addition, evidence is accumulating that an anti-inflammatory diet (along with medication therapy) may be helpful.
Having rheumatoid arthritis often means that you have to pay special attention to the way you move. An occupational therapist or physical therapist can offer suggestions and guidance as you manage ordinary tasks around your home and work. In addition, a therapist can provide special devices that can help you conserve energy and protect your joints during your daily activities. A splint, brace, sling or Ace bandage worn when your joints are especially tender can take the pressure off the joints and protect them from injury. A podiatrist may provide shoe inserts (orthotics) or even suggest surgery to improve pain and function in arthritic feet.
Surgery
In some cases, surgery is needed to remove inflamed tissue, or to reconstruct or replace the affected joint. When rheumatoid arthritis causes significant destruction and pain in the hip or knee, arthroplasty, a surgical procedure to replace the joint, may be an effective option. Because rheumatoid arthritis may cause tendon damage, especially in the hand and wrist, surgical tendon repair may be recommended.
When to call a professional
Tell your doctor if you experience any of the following:
- pain, stiffness, warmth, redness, or swelling at the joints (of the wrist, fingers, neck, shoulders, elbows, hips, knees, ankles, and feet), especially if symptoms are prolonged
- fatigue
- unexplained fever
- pain or stiffness in the morning (lasting more than 30 minutes).
Prognosis
Early, effective treatment can help you live well with rheumatoid arthritis, although the severity of the disease and its response to therapy are highly variable.
Additional info
American College of Rheumatology
http://www.rheumatology.org/
Arthritis Foundation
http://www.arthritis.org/
National Institute of Arthritis and Musculoskeletal and Skin Diseases
https://www.nih.gov/about-nih/what-we-do/nih-almanac/national-institute-arthritis-musculoskeletal-skin-diseases-niams
American Academy of Orthopaedic Surgeons
http://www.aaos.org/
About the Reviewer

Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.