Harvard Health Blog
Can probiotics help treat depression and anxiety?
There is a lot of interest right now in the human microbiome (the populations of bacteria that live in various parts of the body, including the intestine, skin, and lungs). We now know that there are approximately 10 times as many bacterial cells as human cells in the body. The vast majority of these bacterial cells are in the intestinal tract, and they serve many purposes, including digesting foods, manufacturing certain vitamins (for example, vitamin K), and regulating our immune system. Researchers are actively studying whether changes in intestinal bacteria can increase the risk of chronic illnesses, such as obesity or inflammatory bowel disease.
Is the way to your brain through your stomach?
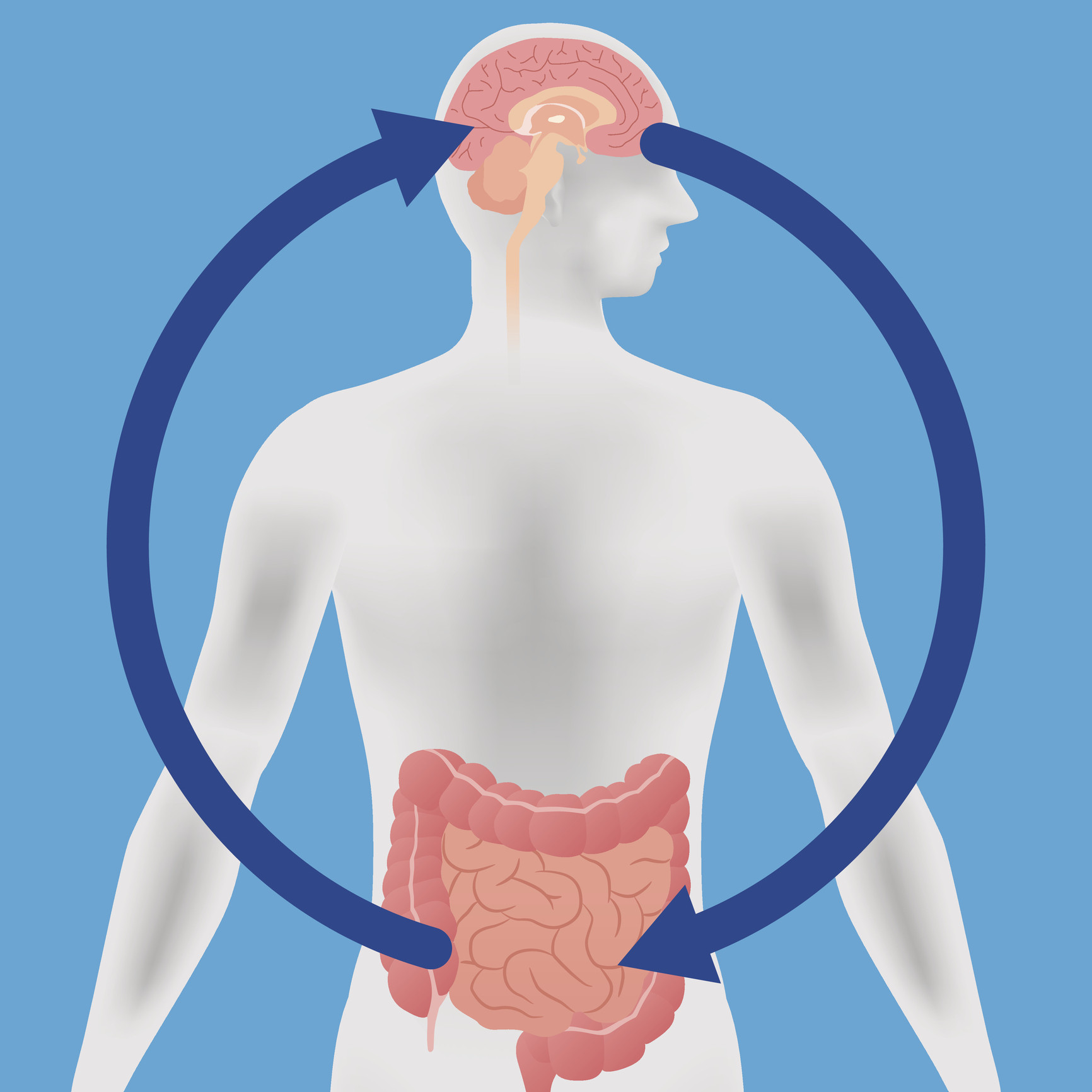
Interest is also developing in the so-called "brain-gut axis." It has been theorized that changes in intestinal bacteria may play a role in neuropsychiatric conditions such as anxiety or depression. The intestine has its own separate nervous system, and generates many of the same neurotransmitters (including acetylcholine and serotonin) that the brain generates. These neurotransmitters are very important in promoting gut motility, and too much or too little of them may result in constipation or diarrhea. Similarly, we believe that the brain and the gut can talk to each other. Therefore, it is possible that anxiety and depression may trigger abdominal pain or other GI symptoms. It is also possible that gastrointestinal conditions such as chronic abdominal pain or constipation might also result in anxiety or depression.
Can probiotics treat chronic conditions (physical and mental)?
If, in theory, bacteria have a role in these chronic conditions, perhaps changing the intestinal bacteria by adding probiotics ("good bacteria") might help treat chronic illnesses. Probiotics have been utilized widely in countries like China and Japan for decades, primarily in the form of fermented milk. In addition, there are a number of animal studies that suggest probiotics may be helpful for conditions like diarrhea or colitis. Unfortunately, probiotics have not yet been shown to treat much human disease.
A recent article in Annals of General Psychiatry reviewed the currently available medical literature on using probiotics to treat anxiety and depression. The doctors identified 10 studies that were well done (in other words blinded and placebo-controlled), and looked at each study in depth. All of these studies had relatively small numbers of patients, ranging as from as few as 42 to as many as 124. The results of these studies were mixed; some suggested that there may be mild benefits of taking probiotics if you have anxiety or depression while other studies showed no benefit. Overall, the authors concluded "the clinical effects of probiotics on mental health have yet to be studied comprehensively."
The bottom line
While it is tempting to hope that probiotics may be used to treat anxiety or depression, at this point there are no compelling data that suggest a true benefit. Since most probiotics are relatively safe, taking them for this reason probably falls into the "doesn't hurt, and might help" category. However, probiotics are probably not a substitute for standard care such as cognitive behavioral therapy, or FDA-approved drugs to treat depression or anxiety. More research as needed in the future, that should try to identify which strains of bacteria are the most effective and the best dose of bacteria to take to treat these conditions.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.















