Harvard Health Blog
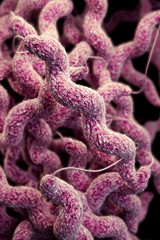
Drug-resistant bacteria a growing health problem
Antibiotic-resistant bacteria sicken more than two million Americans each year and account for at least 23,000 deaths. The main cause? Overuse of antibiotics.
A new report from the Centers for Disease Control and Prevention, Antibiotic Resistance Threats in the United States, 2013, details the health and financial costs of antibiotic resistance in the United States. In terms of health, antibiotic resistance should be in the CDC’s top 15 causes of death. It also adds as much as $20 billion in direct health-care costs. And the problem could get worse before it gets better.
“Antibiotic resistance is rising for many different pathogens that are threats to health,” said CDC Director Tom Frieden, M.D., in a prepared statement. “If we don’t act now, our medicine cabinet will be empty and we won’t have the antibiotics we need to save lives.”
Those are some very strong words from the director of the CDC. Like many doctors and citizens around the country, I am keenly aware of the risks of antibiotics. Still, Dr. Frieden’s words grabbed my attention.
Antibiotic resistance explained
What is antibiotic resistance? Here is a simple example. If you get a strep throat and take penicillin for it, the penicillin will kill off most of the streptococcal (strep) bacteria. But a few strep bacteria might survive. These survivors are, for many different reasons, resistant to the medicine. The next time around, your strep throat might not respond to penicillin.
You can acquire drug-resistant bacteria in many different ways. They can come from overusing antibiotics, or taking them when they aren’t necessary, as for a viral infection. You can develop resistance to antibiotics by eating meat treated with antibiotics. It’s also possible to get an antibiotic-resistant infection from other people—even, unfortunately, from health care professionals.
Why is antibiotic resistance a problem? The major issue is that commonly used antibiotics will become less able to treat common infections. That means doctors must turn to more powerful and sometimes less friendly antibiotics, or may not have anything in their arsenal.
In its report, the CDC identified three types of bacteria as urgent hazards:
- Clostridium difficile. These bacteria can cause severe diarrhea, especially in older people and those who have serious illnesses.
- Enterobacteriaceae. These bacteria, which normally live in the digestive tract, can invade other parts of the body, like the urinary tract, and cause infections.
- Neisseria gonorrhoeae. These bacteria cause gonorrhea, a sexually transmitted infection.
Many other bacteria were listed as “serious” or “concerning” threats. They included some very common bacteria that cause pneumonia and strep throat. Fungi that cause some common yeast infections also made the “serious” list.
The CDC took the opportunity to unveil a four-pronged approach to monitor and address the problem. It aims to:
- prevent infections and the spread of antibiotic resistance
- track antibiotic-resistant infections around the country
- improve how doctors, patients, farmers, and others use antibiotics, and avoid their overuse
- develop new antibiotics and tests to detect antibiotic resistance
Taking action
Everyone can help decrease the impact of antibiotic resistance and slow its growth—or even turn it around altogether. Preventing infection in the first place is important. Here are some steps:
- Decrease excess use of antibiotics. Know when antibiotics do and don’t work. Don’t demand antibiotics from your doctor. Ask whether they will make a difference for your symptoms. The CDC’s Get Smart campaign offers tips and tools.
- Prevent infections. Hand washing (with regular, not antibacterial, soap) is a great way to prevent all infections. Other hygiene measures also are important. For example, sneeze into your elbow, not your hand. Hospitals can reduce risk with thoughtful infection control measures and programs.
- Stay up to date with your vaccinations. Getting vaccinated against pneumonia can help decrease resistance to the very common pneumococcus bacteria.
- Practice safe sex. Use condoms to help prevent the spread of sexually transmitted diseases.
- Learn more about antibiotic use in our food chain. These drugs also can increase antibiotic resistance. Make informed decisions about the food you are buying.
I hope this important report is the beginning of a serious campaign against antibiotic resistance. If these ideas work, then we may see decreased resistance and infections. If they don’t, then we’re heading down a worrisome path in our ability to confront serious, life-threatening infections.
About the Author

Lori Wiviott Tischler, MD, MPH, Assistant Professor of Medicine, Harvard Medical School
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.















