Menopause-related hot flashes and night sweats can last for years

How long do hot flashes last? It used to be said that menopause-related hot flashes fade away after six to 24 months. But for many women, hot flashes and night sweats often last a lot longer—by some estimates seven to 11 years.
The hormonal roller coaster that comes as a woman’s childbearing years wind down can trigger a range of hot flash symptoms. As many as 80% of women going through menopause experience hot flashes. Hot flashes, also known as vasomotor symptoms, are often described as a sudden sensation of heat in the chest, face, and head followed by flushing, perspiration, and sometimes chills. Hot flashes and sweats that occur during sleep can make it hard to get a good night’s rest. The estimates of the duration of these symptoms come from the Study of Women’s Health Across the Nation (SWAN), a long-term study of women of different races and ethnicities who are in the menopausal transition.
"The data from this study confirm what many women already know firsthand. Hot flashes can go on for years and take a toll on a woman’s health and well-being," says Dr. JoAnn Manson, professor of women’s health at Harvard Medical School and professor of epidemiology at Harvard School of Public Health.
The SWAN researchers found that some women are more likely to deal with long-term hot flashes than others. Women who had their first hot flashes before their menstrual periods ended had hot flashes for an average of nine to 10 years. When hot flashes didn’t start until after the last menstrual period, the average duration was only about three and a half years. But even on the short end of the spectrum, that’s a long time to deal with hot flashes and night sweats.
Women in the SWAN study who experienced hot flashes for a longer time tended to be current or former smokers, overweight, stressed, depressed, or anxious. Ethnicity also played a role. African American women reported the longest duration of hot flashes (averaging more than 11 years), while Japanese and Chinese women had hot flashes for about half that time.
The "reality check" the SWAN study provides on hot flashes should encourage women to seek solutions. If hot flashes and night sweats are really bothering you, don’t put up with them. Talk with your doctor about treatment options.
The most effective hot flashes treatment is estrogen-based hormone therapy, though it comes with several downsides. While hormone therapy is very effective at relieving hot flashes, women at older ages have higher risks of stroke, blood clots, and other health problems. "So, it’s important that women explore a full range of treatment options — especially women likely to have persistent hot flashes," advises Dr. Manson.
Several non-hormonal medications can also help relieve hot flashes and night sweats. These include some types of antidepressants, some drugs commonly prescribed for nerve pain, and some high blood pressure medications. As with any medication, it’s best to opt for the lowest dose that effectively relieves your symptoms, and to take it for the shortest amount of time possible.
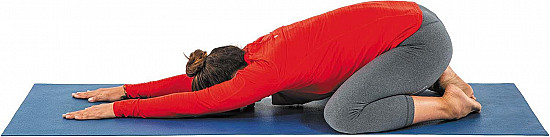
For some women, non-medication measures can help. These include deep-breathing exercises when a hot flash starts; dressing in layers; lowering the thermostat; staying away from caffeine, alcohol, hot beverages, and spicy foods; stress reduction techniques like meditation and mindfulness; and doing your best to stay cool in general.
A free mobile app called MenoPro, helps women understand their treatment options and work with their healthcare providers to find personalized approach for relief. More information is available at the North American Menopause Society website.
About the Author

Nancy Ferrari, Editor in Chief, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.