Harvard Health Blog
The opioid crisis and physician burnout: A tale of two epidemics
In April, the U.S. Surgeon General, Dr. Vivek Murthy, attended a meeting of the Association of Health Care Journalists. In an exclusive interview with MedPage Today, he shared his mounting concerns about two matters: the impact of burnout on physicians and our society’s current opioid crisis. Dr. Murthy stated that he views physicians as being an essential part of the solution to the epidemic of drug overdoses, which have exceeded motor vehicle accidents as one of the leading causes of death.
Dr. Murthy correctly linked the well-being of health professionals with that of the general public, stating, “As I think about the emotional well-being for our country, I am particularly interested in how to cultivate emotional well-being for healthcare providers. If healthcare providers aren’t well, it’s hard for them to heal the people for whom they are caring.”
As the director of Physician Health Services (PHS), an independent non-profit dedicated to promoting and supporting the health and well-being of some 45,000 physicians and medical students in Massachusetts, I have witnessed first-hand how stress and burnout among practicing physicians may play a role in the opioid epidemic.
In the past, physician health programs across the country focused on assisting doctors with drinking problems, drug addiction, and mental illness. Although these conditions continue to challenge a subset of practicing physicians, the rising tide in the physician health world is occupational stress, burnout, and an overall failure to thrive, which may be both personal and professional. Indeed, a recent study on physician burnout published in the Mayo Clinic Proceedings demonstrated that more than half of all physicians are experiencing professional burnout. As burnout increases, satisfaction with work-life balance drops. The data indicate that internists and family medicine physicians, those who prescribe the lion’s share of opioids, are particularly beleaguered — and this conforms to my own experience assisting distressed physicians who are failing to thrive.
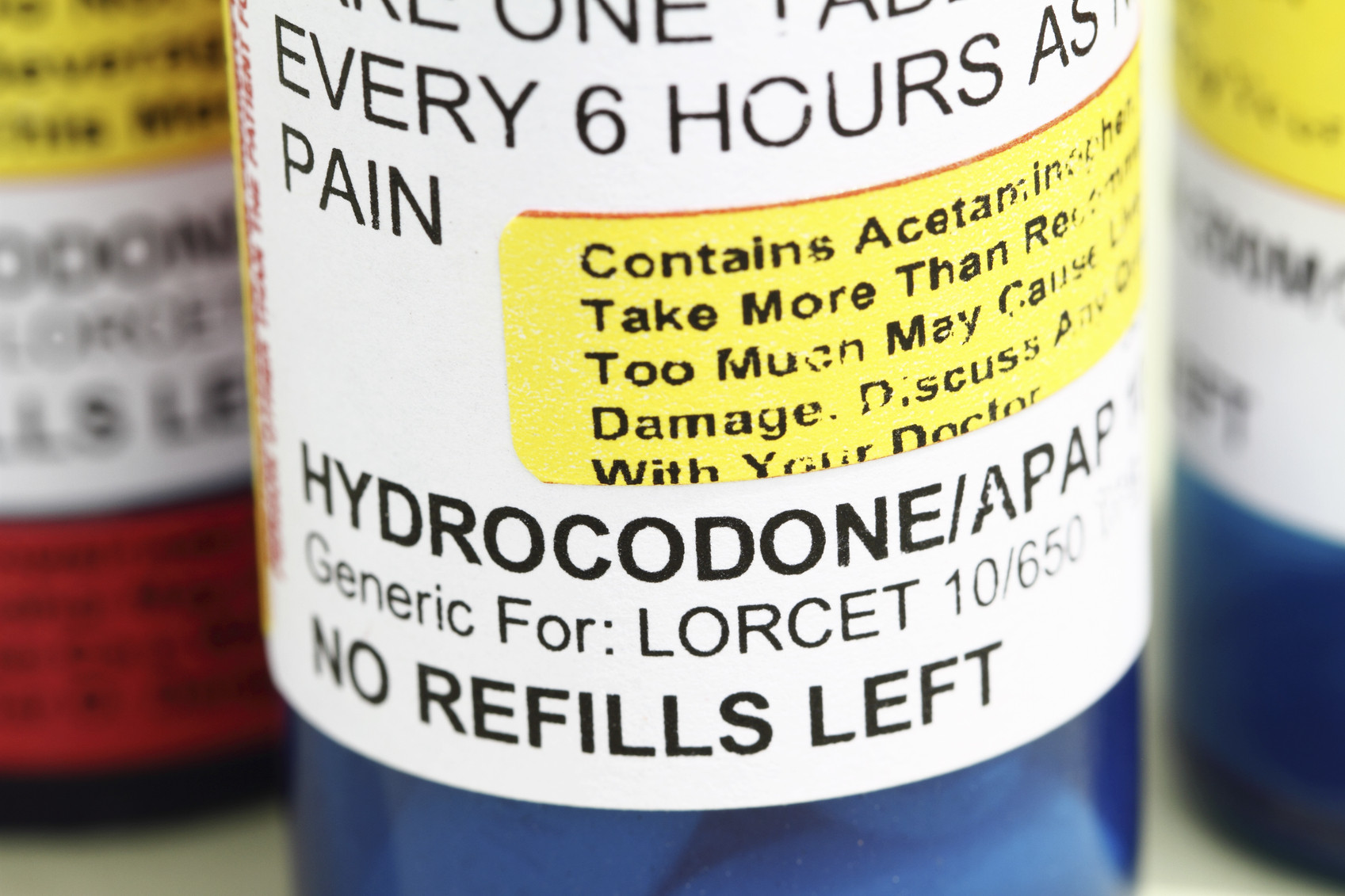
Many physicians in busy primary care practices feel like they are playing a never-ending game of “Whack-a-Mole.” They answer to a growing cadre of masters: faceless managed-care bureaucrats; managers; IT consultants; quality measurement gurus; and…patients. As time grows scarcer and the rewards leaner, being an excellent physician while managing one’s life outside of the office has become increasingly challenging. Given these pressures and demands coming from so many quarters, some adult primary care physicians may not possess enough time or the requisite emotional fortitude to fully explore non-opioid alternatives when, for example, a patient with chronic lower back pain reports that 80 mg of oxycodone (Oxycontin) per day has allowed him to continue working and providing for his family. Scenarios like this raise the possibility that physician burnout may be playing a role in the opioid epidemic.
Solving the burnout crisis of adult primary care physicians is beyond the scope of this blog post. But until our society and the medical profession begin to address this crisis in a vigorous and meaningful way, our quest to put an end to the opioid epidemic remains daunting.
About the Author

Steven A. Adelman, MD, Contributor
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.















