Preventing ovarian cancer: Should women consider removing fallopian tubes?
New recommendations highlight potential benefits.
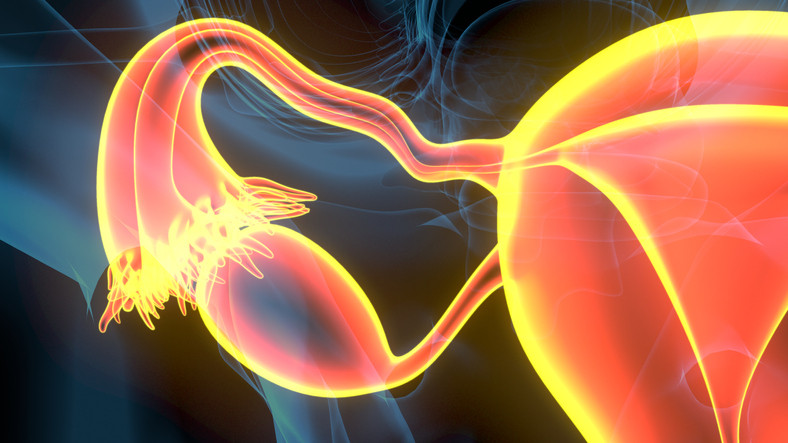
Should a woman consider having her fallopian tubes removed to lower her risk for developing ovarian cancer? Recent recommendations from the Ovarian Cancer Research Alliance (OCRA), endorsed by the Society for Gynecologic Oncology, encourage this strategy, if women are finished having children and would be undergoing gynecologic surgery anyway for other reasons.
Why is this new guidance being offered?
Ovarian cancer claims about 13,000 lives each year, according to the American Cancer Society. The new guidance builds on established advice for women with high-risk genetic mutations or a strong family history of ovarian cancer.
This idea isn't new for women at average risk for ovarian cancer, either: in 2019, the American College of Obstetricians and Gynecologists (ACOG) floated this strategy in a committee opinion.
A Harvard expert agrees the approach is sound, considering established evidence that many cases of aggressive ovarian cancers arise from cells in the fallopian tubes.
"We've known for a long time that many hereditary cases of ovarian cancer likely originate in lesions in the fallopian tubes," says Dr. Katharine Esselen, a gynecologic oncologist at Beth Israel Deaconess Medical Center. "Although we group all of these cancers together and call them ovarian cancer, a lot actually start in the fallopian tubes."
Can ovarian cancer be detected early through symptoms or screening?
No — which helps fuel these recommendations.
Ovarian cancer is notoriously difficult to detect. Symptoms tend to be vague and could be related to many other health problems. Signs include bloating, pelvic pain or discomfort, changes in bowel or bladder habits, feeling full earlier when eating, fatigue, unusual discharge or bleeding, and pain during sex.
Disappointing results from a large 2021 study in the United Kingdom reported in The Lancet show that lowering the risks of a late-stage diagnosis isn't easy. The trial tracked more than 200,000 women for an average of 16 years. It found that screening average-risk women with ultrasound and a CA-125 blood test doesn't reduce deaths from the disease. By itself, the CA-125 blood test isn't considered reliable for screening because it's not accurate or sensitive enough to detect ovarian cancer.
Only 10% to 20% of patients are diagnosed at early stages of ovarian cancer, before a tumor spreads, Dr. Esselen notes. "There's never been a combination of screenings that has reliably identified the majority of these cancers early, when they're more treatable," she says.
What does it mean to be at higher risk for ovarian cancer?
Family history is the top risk factor for the disease, which is diagnosed in nearly 20,000 American women annually. A woman is considered at higher risk of ovarian cancer if her mother, sister, grandmother, aunt, or daughter has had the disease.
Additionally, inherited mutations in the BRCA1 or BRCA2 gene raise risk considerably, according to the National Cancer Institute. (These mutations are more common among certain groups, including people of Ashkenazi Jewish heritage.) While about 1.2% of women overall will develop ovarian cancer in their lifetime, up to 17% of those with a BRCA2 mutation and up to 44% with a BRCA1 mutation will do so by ages 70 to 80.
How much can surgery lower the odds of ovarian cancer?
It's not clear that all women — even those not scheduled for surgery — should undergo removal of their fallopian tubes to reduce this risk once they finish having children, Dr. Esselen says. This surgery can't totally eliminate the possibility of ovarian cancer — and surgery carries its own risks. She recommends discussing options with your doctor depending on your level of risk for this disease:
For those at average risk for ovarian cancer: Available data seem to support the idea of removing the fallopian tubes. Studies of women who underwent tubal ligation ("tying the tubes") or removal to avoid future pregnancies indicate their future risks of ovarian cancer dropped by 25% to 65% compared to their peers. And if a woman is already undergoing gynecologic surgery, such as a hysterectomy, the potential benefits likely outweigh the risks.
Before menopause, removing the fallopian tubes while leaving the ovaries in place is preferable to removing both. That's because estrogen produced by the ovaries can help protect against health problems such as cardiovascular disease and osteoporosis. Leaving the ovaries also prevents suddenly experiencing symptoms of menopause.
"The fallopian tubes don't produce any hormones and aren't really needed for anything other than transporting the egg," she says. "So there's little downside to removing them at the time of another gynecologic procedure if a woman is no longer interested in fertility."
For those at high risk for ovarian cancer: "In a world where we don't have good screening tools for ovarian cancer, it makes sense to do something as dramatic as surgery to remove both ovaries and fallopian tubes when a woman is known to be at higher risk because of a strong family history or a BRCA gene mutations," Dr. Esselen says.
Currently, preliminary evidence suggests it may be safe to proactively remove the fallopian tubes while delaying removal of the ovaries to closer to the time of menopause to avoid an early menopause. However, it's unclear how much this procedure lowers the odds of developing ovarian cancer.
"Generally, the findings so far have focused on the safety of the surgery itself and women's quality of life," Dr. Esselen says. "Long-term data in high-risk women takes a great number of years to accumulate. We need this data to know whether removing the fallopian tubes alone is equally effective in preventing ovarian cancer as removing the tubes and ovaries."
Discussing your options is key
Ultimately, Dr. Esselen says that she advocates OCRA's new recommendations. "For anyone who's completed childbearing, if I'm doing surgery that wouldn't necessarily include routinely removing their fallopian tubes, I'm offering it," she says. "A woman and her doctor should always discuss this at the time she's having gynecologic surgery."
About the Author

Maureen Salamon, Executive Editor, Harvard Women's Health Watch
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.















