Sex and the prostate: Overcoming erectile dysfunction when you have prostate disease

By Harvard Prostate Knowledge
If you are concerned about erectile function, it's important to understand what erectile dysfunction really is. Failing to have an erection one night after you've had several drinks — or even for a week or more during a time of intense emotional stress — is not erectile dysfunction. Nor is the inability to have another erection soon after an orgasm. Nearly every man occasionally has trouble getting an erection, and most partners understand that.
Erectile dysfunction is the inability to attain and maintain an erection sufficient for sexual intercourse at least 25% of the time. The penis doesn't get hard enough, or it gets hard but softens too soon. The problem often develops gradually. One night it may take longer or require more stimulation to get an erection. On another occasion, the erection may not be as firm as usual, or it may end before orgasm. When such difficulties occur regularly, it's time to talk to your doctor.
Erectile dysfunction can have many causes, including some forms of prostate disease and medications and surgery for prostate cancer. Fortunately, in many cases, this problem can often be effectively addressed. Some men find relief by taking medications to treat erectile dysfunction. If these aren't effective for you, a number of other options, including injections and vacuum devices, are available. The possibility of finding the right solution is now greater than ever.
This article explores why men may develop erectile dysfunction as a consequence of some prostate diseases, and details the current treatment options to restore sexual functioning.
The basics: How an erection occurs
At its most basic level, an erection is a matter of hydraulics. Blood fills the penis, causing it to swell and become firm. But getting to that stage requires extraordinary orchestration of body mechanisms. Blood vessels, nerves, hormones, and, of course, the psyche must work together. Problems with any one of these elements can diminish the quality of an erection or prevent it from happening altogether.
Nerves talk to each other by releasing nitric oxide and other chemical messengers. These messengers boost the production of other important chemicals, including cyclic guanosine monophosphate, prostaglandins, and vasoactive intestinal polypeptide. These chemicals initiate the erection by relaxing the smooth muscle cells lining the tiny arteries that lead to the corpora cavernosa, a pair of flexible cylinders that run the length of the penis (see Figure 1).
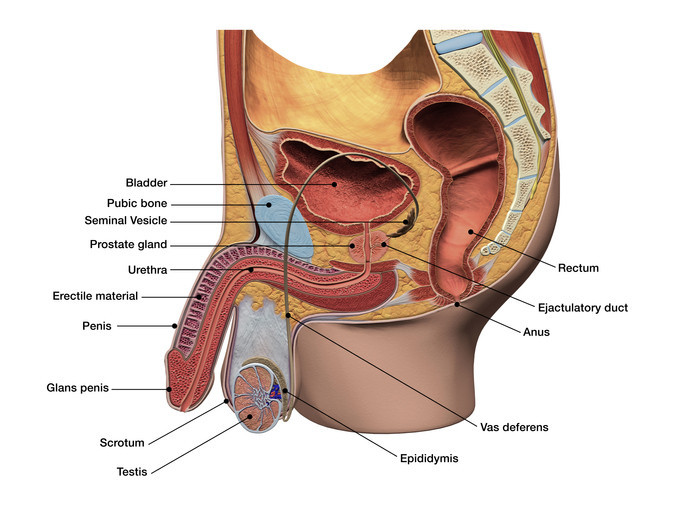
Figure 1: Anatomy of the penis
The penis is made up of three cylindrical bodies, the corpus spongiosum (spongy body)—which contains the urethra and includes the glans (head) of the penis—and two corpora cavernosa (erectile bodies), that extend from within the body out to the end of the penis to support erection. Blood enters the corpora cavernosa through the central arteries. Image: Hank Grebe/Getty Images |
As the arteries relax, the thousands of tiny caverns, or spaces, inside these cylinders fill with blood. Blood floods the penis through two central arteries, which run through the corpora cavernosa and branch off into smaller arteries. The amount of blood in the penis increases six-fold during an erection. The blood filling the corpora cavernosa compresses and then closes off the openings to the veins that normally drain blood away from the penis. In essence, the blood becomes trapped, maintaining the erection.
Obviously, an erection isn't permanent. Some signal — usually an orgasm, but possibly a distraction, interruption, or even cold temperature — brings an erection to an end. This process, called detumescence, or deflation, occurs when the chemical messengers that started and maintained the erection stop being produced, and other chemicals, such as the enzyme phosphodiesterase 5 (PDE5), destroy the remaining messengers. Blood seeps out of the passages in the corpora cavernosa. Once this happens, the veins in the penis begin to open up again and the blood drains out. The trickle becomes a gush, and the penis returns to its limp, or flaccid, state.
It's usually difficult for a man to get another erection right away. The length of the interval between erections varies, depending on a man's age, his health, and whether he is sexually active on a regular basis. A young, sexually active man in good health may be able to get an erection after just a few minutes, whereas a man in his 50s or older may have to wait 24 hours. One reason may be that nerve function slows with age.
Indeed, erections may work on a use-it-or-lose-it principle. Some research suggests that when the penis is flaccid for long periods of time — and therefore deprived of a lot of oxygen-rich blood — the low oxygen level causes some muscle cells to lose their flexibility and gradually change into something akin to scar tissue. This scar tissue seems to interfere with the penis' ability to expand when it's filled with blood.
Why erectile dysfunction may result from prostate disease
In the past, it was thought that most cases of erectile dysfunction were psychological in origin, the result of such demons as performance anxiety or more generalized stress. While these factors can cause erectile dysfunction, doctors now think that 70% of the time the problem can be traced to a physical condition that restricts blood flow, hampers nerve functioning, or both. Such conditions include diabetes, kidney disease, multiple sclerosis, atherosclerosis, vascular disease, and alcoholism.
However, some types of prostate disease and treatments (particularly for prostate cancer) may also be responsible.
Prostate cancer
Surgery for prostate cancer can sever some of the nerves or arteries that are needed for an erection. For men who undergo a radical prostatectomy (removal of the prostate gland), the estimates of how many men will regain their ability to have erections vary widely, from 25% to 80%. Even so-called nerve-sparing surgical techniques lead to erectile dysfunction in up to half or more of all cases. The results depend on such variables as a patient's age, the surgeon's skill, and the tumor locations (if a tumor is too close to the nerve bundle, the nerves can't be spared). Even when the nerves are not permanently impaired, it can still take six to 18 months for the tiny nerve fibers to recover from the trauma of surgery and restore sexual function.
Radiation treatment for prostate cancer can also harm erectile tissues. Both external beam radiation and radiation-emitting seeds implanted in the prostate (brachytherapy) lead to erectile dysfunction in about half of men who receive these therapies. However, these changes may not occur for up to two years after treatment.
Erectile dysfunction is sometimes a side effect of some hormone therapy medications prescribed for men with prostate cancer that has spread beyond the prostate. Among such hormone-based medications are leuprolide (Lupron), and goserelin (Zoladex). Others, such as flutamide (Eulexin) and bicalutamide (Casodex) may cause erectile dysfunction to a lesser degree. Even prostate cancer itself, in its advanced stages, can spread to the nerves and arteries that are necessary for an erection.
Benign prostatic hyperplasia
Men who have benign prostatic hyperplasia (BPH), a noncancerous enlargement of the prostate, may also experience erectile dysfunction and ejaculatory problems. Although BPH does not itself cause these problems, some of the treatments used for BPH can do so. For example, finasteride (Proscar), an anti-testosterone drug prescribed for BPH, has been linked to erectile dysfunction in 3.7% of men who use it and to diminished libido in 3.3%. But alpha blockers such as tamsulosin (Flomax), alfuzosin (Uroxatral), and silodosin (Rapaflo) can improve the symptoms of BPH with a lower risk of sexual side effects. Transurethral resection of the prostate, a surgical technique often used when medication fails, also causes erectile dysfunction in a small percentage of men.
Low testosterone
Testosterone levels tend to decrease with age. They peak by early adulthood and then can drop by up to 1% per year beginning around age 40. Sometimes an abrupt fall occurs because of an injury or illness (such as an infection), chemotherapy or radiation treatment, or certain medications.
The hormone testosterone plays a big part in men's health, but perhaps its most meaningful role is to fuel sex drive. If testosterone levels drop too low, men can experience erectile dysfunction as well as lackluster libido.
Prostatitis
This inflammation of the prostate gland can be either acute (usually caused by a bacterial infection) or chronic (usually not caused by an infectious agent). Symptoms include pain during urination, more frequent urination, and — possibly — a discharge from the penis or fever. Severe prostatitis can cause erectile dysfunction directly. In milder forms, the condition can produce painful ejaculation, which can certainly interfere with sexual pleasure and may lead to erectile dysfunction.
Diagnosing erectile dysfunction
If you've been having difficulty getting or sustaining erections, talk about it with your doctor. Such a conversation is never easy, but thanks in part to greater publicity about this problem and its treatment, many obstacles have been toppled.
You may recall the TV commercials that showed self-assured men going to the doctor's office to discuss the problem and emerging relieved after having taken this important step. What's misleading is that such commercials leave the impression that there's not much to discuss — all you need is a prescription and your erections will come back. In reality, your doctor must diagnose the cause of your erectile dysfunction in order to recommend an effective treatment.
While therapy usually does involve medication, erectile dysfunction is sometimes a symptom of an underlying condition that requires its own treatment. Also, medication is more effective for some causes of erectile dysfunction than for others. For instance, if you've had prostate surgery, pills probably won't work as well as other treatments. And if a psychological condition is significantly involved, you may benefit from counseling with a mental health professional trained in sex therapy.
Providing your medical history
At first, the doctor will probably ask you about your medical history. Do you have any chronic illnesses? What illnesses and operations have you had in the past? What medications are you taking, if any? Your doctor is also likely to ask about your psychological well-being and lifestyle: Do you suffer (or have you ever suffered) from depression? Are you under a lot of stress? Do you drink alcohol? Smoke? Use illegal drugs? Have you felt a loss of affection for your partner? Have you recently grown interested in a new partner?
As part of this health history, be prepared to tell your doctor specific details about the symptoms that brought you to the office and when they began. Your doctor might want to know how often you had sex before the problem started and if there have been weeks or months in the past when you've had erectile dysfunction. Your doctor may conduct a written or verbal screening test.
If the cause is clear — a recent operation for prostate cancer, for example — the conversation may move directly to your treatment options. Otherwise, you may need to answer more questions to help the doctor narrow down the possible causes and avoid unnecessary testing.
A key issue is whether the symptoms came on gradually or suddenly. Erectile dysfunction that comes on gradually often points to causes that involve blood flow or nerves. On the other hand, a sudden loss of sexual desire or the ability to have erections usually suggests that a medication or psychological difficulty, such as depression or stress, may be to blame. Don't be embarrassed if the doctor asks you about early morning erections or whether you can achieve an erection if you masturbate. The ability to do so is an important clue in determining whether the problem is psychologically or physically based (see Table 1).
Table 1: Diagnosing the problem |
|
Possible cause of erectile dysfunction |
What the doctor does |
|
Vascular (circulatory system) |
Takes your blood pressure and listens to your heart. Checks pulse in groin and feet. Checks your abdomen for aortic aneurysm. |
|
Neurological (nervous system) |
Tests reflexes of your knees and ankles, as well as anus. Checks for sensation in your legs and feet. |
|
Hormonal (endocrine system) |
Assesses testicular size and breast development. Checks your thyroid gland. |
|
Local (reproductive system) |
Examines your penis for curvature and scarring that may indicate Peyronie's disease. Checks your prostate. |
|
Psychological (stress, anxiety, emotional) |
Assesses the history of the problem, especially whether it started suddenly and if nocturnal erections are affected. |
The physical exam
During the physical exam, the doctor will listen to your heart for signs of a murmur and other abnormalities that can affect blood flow. He or she will also take your blood pressure; both high and low blood pressure can impair blood flow. The doctor will check your pulse in several places — at the wrist, ankle, and groin. Slow or low pulse in any of these areas can mean that not enough blood is reaching tissues in the extremities, including the penis.
In addition, the doctor will examine your testicles, penis, and chest. Abnormally small testicles and enlarged breasts are sometimes signs of inadequate testosterone. Patches of scar tissue felt in the penis suggest Peyronie's disease. Your doctor may check the prostate gland for signs of infection or cancer, by doing a digital rectal exam.
Your checkup will probably include tests for cholesterol (to assess your risk of cardiovascular disease) and triglyceride and blood sugar levels (to check for diabetes). The doctor might also ask for a urine specimen because the presence of red or white blood cells could be a sign of a un underlying urologic problem.
Tests
Now that medication can successfully treat most men with erectile dysfunction, many once routine diagnostic tests are used only when the doctor suspects the patient has an underlying problem requiring additional treatment.
Hormone tests. Checking testosterone levels used to be one of the first tests ordered for men with erectile difficulty, but that was before doctors realized that testosterone deficiency was rarely the source of the problem. Now, hormone testing is done for men whose medical exams suggest an endocrine problem and for those who have experienced a loss of sexual desire.
Your doctor also may want to check your blood levels of prolactin (a pituitary hormone that can block the action of testosterone) or thyroid–stimulating hormone (a good indicator of an under-active or overactive thyroid gland).
Blood flow tests. A color duplex Doppler ultrasound, an imaging technique, can reveal problems with blood flow through the arteries or veins of the penis, such as venous leakage. A newer version, called penile Doppler, can be done in a physician's office. If you've tried pills for erectile dysfunction but haven't found them helpful, your doctor may inject prostaglandin, a fatty acid that widens blood vessels, into your penis to see if this causes an erection. If so, there's a good chance that you will respond to one or more of the injectable drugs used to treat erectile dysfunction.
Nocturnal tumescence tests. If it's unclear whether your erectile difficulties have a psychological or a physical cause, your doctor may suggest a nocturnal penile tumescence test. Psychological factors come into play when you're trying to achieve or maintain an erection. But the psyche doesn't affect nocturnal erections, which occur involuntarily during sleep. Physical causes affect both kinds of erections.
Table 2: Comparing the temporary treatments |
|||||
|
Therapy |
Onset of action |
Duration of effectiveness |
Advantages |
Disadvantages |
|
|
sildenafil (Viagra) |
30–60 minutes |
4–5 hours |
Oral medication, very effective (about 70%), few side effects |
Cannot be used by men taking nitrates or those with unstable cardiovascular disease |
|
|
vardenafil (Levitra) |
15–30 minutes |
4–5 hours |
|||
|
tadalafil (Cialis) |
30–45 minutes |
24–36 hours |
|||
|
Avanafil (Stendra)
alprostadil injections (Caverject, Edex) |
15–30 minutes
5–20 minutes |
6 - 12 hours
30–60 minutes |
Highly effective (about 80%), few side effects |
Requires training; injections unpleasant for many men; may cause penile pain or painful sustained erections (priapism) |
|
|
alprostadil pellets (MUSE) |
5–15 minutes |
30–60 minutes |
Moderately effective (about 30%) |
Requires training; may cause penile pain, usually mild; may cause dizziness |
|
|
vacuum pump |
Immediate |
While in use |
Highly effective (about 80%), no serious side effects |
Requires training; cumbersome and awkward; may cause penile numbness or bruising |
|
|
penile band |
Immediate |
While in use |
Effective when used properly, helpful for men with venous leakage who cannot sustain an erection |
May be awkward to use |
|
Treating erectile dysfunction
If you are diagnosed with erectile dysfunction, you have a number of treatment options.
PDE5 inhibitors: Viagra, Levitra, and Cialis
Approved by the FDA in 1998, sildenafil (Viagra) revolutionized the way we think about — and treat — erectile dysfunction, largely because it is so easy to use and effective. Since then the FDA has approved three closely related drugs, vardenafil (Levitra), avanafil (Stendra) and tadalafil (Cialis).
All four drugs work in a similar fashion, by affecting the normal physiology of the penis. In particular, they block PDE5, an enzyme that breaks down the erection-producing chemical cyclic guanosine monophosphate. This enables the penis to fill with blood and to stay erect long enough for intercourse. Of course, it's important to realize that none of these drugs is an aphrodisiac. You've got to feel sexually stimulated in order for them to work.
The main differences between the drugs have to do with timing: how quickly they begin to work, and how long their effects last (see Table 2). Levitra may start working slightly faster than Viagra (within a half-hour instead of an hour) although the FDA says that like Viagra, it should be taken about an hour before sexual activity. Some studies suggest that Levitra may help some men who don't respond to Viagra. And while some doctors are skeptical about this claim, there's no harm in trying Levitra or Cialis if Viagra doesn't work for you.
Cialis stays active in the body much longer than the other drugs. Viagra and Levitra last about 4 to 5 hours (and sometimes up to 12 hours). But with Cialis, the window of opportunity ranges from 24 to 36 hours, which is why it's sometimes called "the weekend drug." Another minor difference is that while Viagra's action may be delayed or impaired when taken with food (especially high-fat foods), that's not the case with Levitra or Cialis.
Cialis has also been approved to treat men with both erectile dysfunction and BPH. The dose is lower, usually 5 milligrams per day.
Side effects. So far, the risks and side effects of these three drugs seem to be roughly the same. They all work by relaxing smooth muscle cells, which widens blood vessels — primarily in the penis, but also in other parts of the body. The most common side effect is a headache, which occurs in about 16% of users. Other reactions include flushing, upset stomach, nasal congestion, and urinary tract infections. But when the drugs are used properly, these side effects are relatively mild, and most disappear after a few hours. In rare cases, some men experience temporary, mild visual problems, mainly seeing a blue tinge, but also increased sensitivity to light and blurred vision. However, men with retinitis pigmentosa, a rare eye disease, should be very cautious about using these medications.
Drug interactions. Within several hours of taking PDE5 inhibitor drugs, blood pressure tends to drop slightly: The top (systolic) number dips 8–10 mm Hg, while the bottom (diastolic) number goes down by 5–6 mm Hg. So it's very important to avoid taking these drugs with medications that contain nitrates, which also lower blood pressure. Interactions between these two types of drugs can cause life-threatening drops in blood pressure. (The nitrates and nitrites found in food don't pose a problem.) Men who take long-acting nitrates, including isosorbide dinitrate (Isordil, Sorbitrate, and others) and isosorbide mononitrate (Imdur, Ismo, and others), or who use nitroglycerine patches or paste should not take PDE5 inhibitor drugs. And they should not use short-acting, under-the-tongue tablets or a spray form of nitroglycerine within 24 hours of taking either Viagra or Levitra. For Cialis, the ban extends to 48 hours.In 2005, reports linked Viagra use to another rare eye disease, non-arteric anterior ischemic optic neuropathy, which can lead to blindness. These reports serve as a reminder to men over 50 to get regular eye check-ups and to alert a physician to any unusual vision problems after taking a PDE5 inhibitor drug.
Men who take medications known as alpha blockers should be cautious about taking PDE5 inhibitors. If you take an alpha blocker, ask your doctor before taking any PDE5 inhibitor. For example, Viagra shouldn't be taken within four hours of taking an alpha blocker.
Other considerations. Although the PDE5 inhibitors are expensive, many health insurance plans (including Medicare) cover them, although most have a limit of four pills per month. Perhaps even more important considerations are the sometimes complicated and unexpected challenges that these medications may present to your sexual relationship. Some partners who've grown comfortable in a relationship without intercourse may need time to shift gears, so to speak, if the drug is successful. Use of these drugs may raise other issues for couples. Should you tell your partner before or after you've started taking it? Will this put pressure on your partner to have sex? Should you take the medication and just hope your partner will be in the mood? The best way to address these questions is to talk about them with your partner. Particularly if you're in an established relationship, your partner should know that you have a prescription for one of the drugs, and the two of you can decide together how and when to use it.
Injections
What if PDE5 inhibitors don't work for you? Many men who can't use these drugs or find them ineffective are able to get erections by injecting one or more prescription drugs into the side of the penis. The very idea may make you squeamish, and it's certainly not as easy as taking a pill. But the needle isn't very big (about half an inch long, the same size as those used to inject insulin), and drug injections can produce results.
Indeed, for men whose erectile dysfunction is caused by diabetes, injection therapy is more effective than Viagra. And it's the single most effective treatment available for men who experience the problem as a result of prostate surgery. Many men learn the technique quickly after a demonstration by a doctor or nurse in the doctor's office
The main side effects of the injections are mild to moderate pain, bruising, or scarring. Like Viagra, injectable drugs can also cause low blood pressure. Although rare, this side effect is most likely to occur if a man takes too large a dose or if he injects himself more than once in 24 hours.There are several injectable drugs, all of which work by relaxing the smooth muscle tissue of the penis and allowing blood to flow into the corpora cavernosa. The only one specifically approved for erectile dysfunction is the prostaglandin alprostadil (Caverject, Edex). However, a number of older drugs that were approved for other uses may be considered. For example, a preparation called Trimix contains a mixture of papaverine, phentolamine, and alprostadil.
Another rare complication is priapism, an erection that lasts too long. Any man who has an erection that lasts for more than three hours after an injection should go to an emergency room. An erection that lasts longer than six hours can cause scarring and complete loss of erectile function. Because of these potential side effects, doctors prescribe the lowest effective dose. A doctor or nurse usually gives a patient an injection in the office to establish what that dose is before writing a prescription.
If you're using injectable drugs, there are some things you can do to help the therapy feel more natural for you and your partner. One is to take a low dose and ask your partner for manual or oral stimulation to help achieve a full erection. That way, your partner will feel more involved. You might also suggest that your partner watch you inject yourself once or twice to help overcome any initial discomfort with the process. But if you're more comfortable doing this privately, that's fine, too. What's most important for the treatment's success — and for your emotional well-being — is that you and your partner feel at ease with it.
MUSE therapy
In addition to being available as an injectable drug, alprostadil comes in the form of tiny pellets designed to be inserted into the penis shortly before intercourse. The pellet form is an alternative to injections. These pellets are part of a therapy called "medicated urethral system for erection," but your doctor will probably just use the acronym MUSE. This method of treatment uses a disposable plastic applicator to insert a pellet about an inch into the urethra. From there, the drug is quickly absorbed by the surrounding tissue and reaches the corpora cavernosa, where it dilates the arteries.
Devices to help achieve or maintain an erectionThough an early study reported that MUSE enabled 65% of men to have intercourse successfully at least once, clinical experience has shown that it is effective in only about 30% of men. Although some men consider MUSE easier to use than injections, about 10% of those who try it find the application process mildly painful, and about 3% become dizzy and develop low blood pressure. Because of the risk of low blood pressure, you should not use MUSE more than twice in 24 hours. Like injectable drugs, MUSE is available only by prescription and must first be used in the doctor's office to determine the lowest effective dose.
If none of the medications are helpful or appropriate for you, or if you just don't want to use them, there are other options. In particular, you can turn to a number of different devices to produce or maintain an erection.
Penile band. A penile band may help men who can get an erection but can't sustain it because of venous leakage. These ring-like devices, which don't require a prescription, fasten around the base of the erect penis to keep blood from escaping. Penile bands are completely effective when used properly.
Vacuum erection devices. Until prescription medications came along, the only proven at-home therapy for erectile dysfunction involved using a vacuum pump. With this therapy, you lubricate your penis and put it into an airtight plastic cylinder that's attached to a handheld pump. Some pumps are manual, while others operate on a battery. In either case, air is pumped out of the cylinder to create a vacuum, which increases blood flow to the penis. Once an erection occurs, which usually takes about five minutes, you remove your penis from the cylinder and fit a rubber ring around the base of the penis to prevent blood from draining away. The erection lasts until the ring is removed.
In addition, the erection doesn't feel as natural as one produced by a drug. Although firm, the erection can be somewhat floppy because it starts above the base of the penis. About 10% of men have side effects, such as pain, bruising, or difficulty ejaculating, any of which can cause discomfort during sexual activity. Also, these pumps are not an option for men with blood disorders, such as blood-clotting irregularities or leukemia.Vacuum pumps are noninvasive and highly effective, working for about 80% of men. Their advantage over medication is that they can be used as often as a man wants. But there are several disadvantages. Having to fuss with the pump can interrupt lovemaking. And some men find the pumps difficult to use.
Surgical implants
Surgical implants should be considered only after you've tried other, less invasive options. Penile implants date back to the 1930s, when a piece of human rib was surgically placed inside a man's penis. Since then, the process has been refined, and now there are two kinds of implants.
Silicone rods. One type of implant consists of two pencil-thin silicone rods that are placed in the penis above the urethra. The operation is done on an outpatient basis and takes about an hour. The penis remains permanently erect, although it can be pointed down along the thigh to conceal it under clothing.
Inflatable cylinders. Another kind of penile implant consists of two inflatable cylinders positioned in the corpora cavernosa, which produce an erection when filled with saline fluid. The fluid is pumped from a reservoir implanted in the abdomen or the scrotum. Although an inflatable implant produces a more natural erection than a silicone rod, it's more prone to complications, like infections and malfunction. About 5% of men need a second operation to replace the implant.
Vascular surgery
Vascular surgery is used only for men whose erectile dysfunction results from specific blood vessel problems. There are two types of such operations, but neither has a high rate of success. The first — for men whose problem involves the leakage of blood from certain vessels during an erection — ties off those vessels so they retain blood.
The second type of vascular surgery is used when the problem is the blockage of isolated blood vessels. In such cases, the surgery entails bypassing the blocked vessels to allow more blood into the penis. Bypass operations are reserved mainly for patients whose blood flow problems result from injuries such as pelvic fractures. For each of these operations, the success rate in restoring normal erectile function is less than 30%.
Hormone therapy
Testosterone supplements are appropriate only if you have abnormally low levels of this hormone. The supplements can help boost your libido and improve your ability to have erections. These supplements are now nearly always given in gel form, which you apply daily to your shoulders. Other forms are less convenient (doctor-administered injections) or cause skin irritation (skin patches). The exact role that low testosterone plays in erectile dysfunction remains unclear.
Image: laflor/Getty Images
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.