Type 2 diabetes: Which medication is best for me?

If you are living with type 2 diabetes, you certainly are not alone. One in 10 people in the US has diabetes, according to the CDC. However, despite considerable progress in diabetes treatment over the past 20 years, fewer than half of those with diabetes actually reach their target blood sugar goal.
In part, this may be because doctors can be slow to make changes to a patient’s treatment plan, even when a patient’s treatment goals are not being met. One reason for this may be the overwhelming number of medications currently available. And yet, waiting too long to adjust treatment for type 2 diabetes can have long-lasting negative effects on the body that may raise the risk of heart and kidney disease and other complications.
What is type 2 diabetes?
Type 2 diabetes is a chronic disease where the body’s ability to use glucose or sugar as fuel is impaired. Our bodies produce a hormone called insulin which enables sugar from carbohydrates in food we eat to reach the cells and be used as energy. In type 2 diabetes, insulin’s ability to do its job is compromised, and over time the body actually produces less of it. This means less sugar in the cells for fuel, and more sugar in the blood where it can’t be used. Having high levels of blood sugar over time can cause damage to vital organs like the heart, kidneys, nerves, and eyes.
Some risk factors that predispose people to developing type 2 diabetes, such as genetics and age, are not modifiable. Other risk factors, such as being overweight or having obesity, can be altered. This is why losing 5% to 10% of one’s baseline weight by healthful eating and physical activity remains the backbone of type 2 diabetes management.
Most diabetes medications effectively lower blood sugar
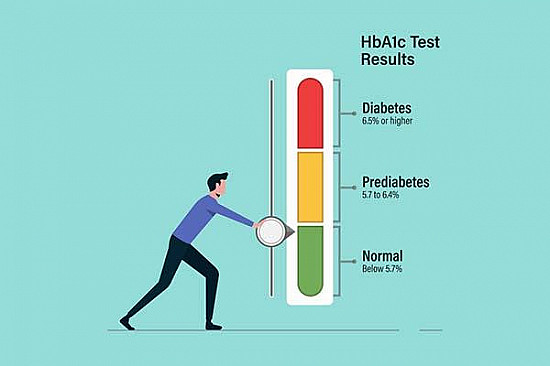
The blood sugar goal for most adults with diabetes is an A1C of below 7%. (A1C is a measure of a person’s average blood sugar over a period of about three months.) In many people, diet and exercise are not enough to reach this goal, and one or more medications may be needed. Metformin is a tried and tested medicine that has been used for many decades to treat type 2 diabetes, and is recommended by most experts as first-line therapy. It is affordable, safe, effective, and well tolerated by most people.
When metformin does not adequately control blood sugar, another medication must be added. It is at this point that doctors and patients must choose among the many drugs and drugs classes available to treat type 2 diabetes. In general, for people who are at low risk of heart disease or have no history of diabetic kidney disease, most diabetes medications that are added to metformin effectively reduce blood sugars and can lower A1C to under 7%.
So, how to choose a medication? Each person with diabetes has their own goals, needs, and preferences. Before choosing a medicine, it is important to ask some relevant questions: Is my blood sugar at goal? Is this medicine affordable? Do I have heart or kidney disease? What are the side effects? Is it a pill or injection, and how often is it taken?
Regardless of which treatment is selected, the American Diabetes Association Standards of Care recommends reassessment of diabetes control every three to six months, followed by modifications to treatment if needed.
Newer diabetes medications: Weighing benefits and risks
Lately, newer treatment options for type 2 diabetes — glucagon-like peptide-1 (GLP-1) receptor agonists and sodium-glucose cotransporter-2 (SGLT2) inhibitors — have been heavily advertised. These newer drug classes lower blood sugar and also have cardiovascular and kidney benefits.
GLP-1 receptor agonists are drugs that lower blood sugar after eating by helping your body’s insulin work more efficiently. All drugs in this group except one are self-injected under the skin, either daily or weekly. Several of them, such as liraglutide (Victoza), semaglutide (Ozempic), and dulaglutide (Trulicity), have been shown to lower the risk of cardiovascular disease in people who are at high risk for it, or who have pre-existing heart disease. They also promote weight loss. Some people who take GLP-1 receptor agonists may have side effects such as nausea and vomiting, and in very rare cases pancreatitis.
SGLT2 inhibitors like empagliflozin (Jardiance), canagliflozin (Invokana), dapagliflozin (Farxiga), and ertugliflozin (Steglatro) are also a newer class of medications that work by blocking your kidneys from reabsorbing sugar back into your body. They also have cardiovascular benefits, especially in those who have heart failure, and have been shown to slow the progression of diabetic kidney disease. Other benefits include lowering blood pressure and promoting weight loss. Use of these medications may increase the risk of genital yeast infections, especially in women. A rare but serious consequence of SGLT2 inhibitors is diabetic ketoacidosis, which is a medical emergency that can be avoided by stopping these medications in consultation with your doctor before major surgeries, or if you are ill or fasting.
While these diabetes medications certainly have more to offer than just improvements in blood sugar, they remain costly and inaccessible to many individuals. This is why it is essential to have an open and honest conversation with your doctor about what is most important to you and what aligns with your goals and preferences. Management of a complex disease like diabetes takes an entire team, with you being the key team member.
About the Author

Samar Hafida, MD, Contributor
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.