Acute sinusitis
- Reviewed by Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
What is acute sinusitis?
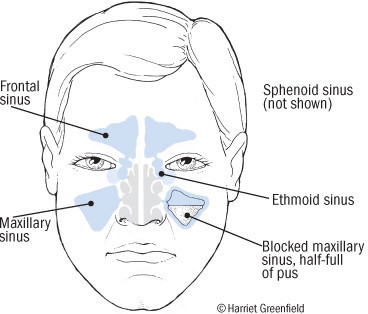
Sinuses are air-filled spaces behind the bones of the upper face: between the eyes and behind the forehead, nose and cheeks. The lining of the sinuses are made up of cells with tiny hairs on their surfaces called cilia. Other cells in the lining produce mucus. The mucus traps germs and pollutants and the cilia push the mucus out through narrow sinus openings into the nose.
When the sinuses become inflamed or infected, the mucus thickens and clogs the openings to one or more sinuses. Fluid builds up inside the sinuses causing increased pressure. Also bacteria can become trapped, multiply and infect the lining. This is sinusitis.

Sinusitis is can be chronic (long-lasting or frequently returning) or acute. Acute sinusitis lasts three weeks or less and the person should have no more than three episodes per year. Acute sinusitis is extremely common. It usually is caused by an upper respiratory viral infection.
The inflammation and swelling of the lining of the sinuses can be triggered by
- Viral infections, such as a common cold
- Allergies
- Air pollution and cigarette smoke
- Dental infections
- Narrowed nasal passages from nasal polyps.
Symptoms of acute sinusitis
Common symptoms of acute sinusitis include nasal congestion, thick green nasal discharge, fever, headache, tiredness and facial pain. Some symptoms depend on which sinus is inflamed. For example:
- Frontal sinusitis (behind the forehead) can cause pain in the forehead and pain that gets worse when lying on your back.
- Ethmoid sinusitis (behind the bridge of the nose) can cause pain between the eyes, eyelid swelling, loss of smell, and pain when touching the sides of the nose.
- Sphenoid sinusitis (behind the eyes) can cause earaches, neck pain or headache at the top of the head or deep behind the forehead.
- Maxillary sinusitis (behind the cheeks) can cause pain in the cheeks, under the eyes, or in the upper teeth and jaw.
Diagnosing sinusitis
A sinus infection can be difficult to diagnose in the early stages because it can mimic a common cold. Both can cause nasal congestion and fatigue. However, a common cold usually will improve in five to seven days, while an untreated sinus infection can last three weeks or longer. Sinus infections also are more likely to cause a green nasal discharge, fever and facial pain.
Your doctor will diagnose acute sinusitis based on your symptoms, medical history and a simple office examination. The doctor will ask about your symptoms and how long they last, look into your ears, nose and throat, and may tap or press on your face to test for tenderness over specific sinuses.
If your doctor is uncertain of your diagnosis, he or she may use other methods to see inside the sinuses. Some physicians may insert a nasopharyngoscope (a thin, lighted tube with a camera on the end) into your nose to look for abnormalities. X-rays and computed tomography scans (CT) also can provide a look at the sinuses, especially those that are deep within the head.
Expected duration of acute sinusitis
By definition, acute sinus infections resolve within three weeks. Infections that last longer than three weeks are considered chronic sinusitis.
Preventing acute sinusitis
There are some measures you can take to decrease your risk of developing sinusitis. If you smoke cigarettes, you should quit. The smoke can irritate nasal passageways and increase the likelihood of infection. Nasal allergies can trigger sinus infections, too. By identifying the allergen (the substance causing the allergic reaction) and avoiding it, you can help prevent sinusitis.
If you have congestion from a cold or allergies, the following may help to reduce the risk of developing sinusitis:
- Drink lots of water. This thins nasal secretions and keeps mucous membranes moist.
- Use steam to soothe nasal passages. Breathe deeply while standing in a hot shower, or inhale the vapor from a basin filled with hot water while holding a towel over your head.
- Avoid blowing your nose with great force, which can push bacteria into the sinuses.
Some doctors advise periodic home nasal washings to clear secretions. This may help prevent, and also treat, sinus infections.
Treating acute sinusitis
Many sinus infections improve without treatment. However, several medications may speed recovery and reduce the chance that an infection will become chronic.
Decongestants — Congestion often triggers sinus infections, and decongestants can open the sinuses and allow them to drain. Several are available:
- Pseudoephedrine (Sudafed) is available without prescription, alone or in combination with other medications in multi-symptom cold and sinus remedies. Pseudoephedrine can cause insomnia, racing pulse and jitteriness. Do not use if you have high blood pressure or a heart condition.
- Oxymetazoline (Afrin, Dristan and others) and phenylephrine (Neo-Synephrine and others) are found in nasal sprays. They are effective and may be less likely to cause the side effects seen with pseudoephedrine. However, using a nasal decongestant for more than three days can cause worse symptoms when you stop the medication. This is called the rebound effect.
Antihistamines — These medications help to relieve the symptoms of nasal allergies that lead to inflammation and infections. However, some doctors advise against using antihistamines during a sinus infection because they can cause excessive drying and slow the drainage process. Many over-the-counter antihistamines are available as brand name products and less expensive generic versions.
Nasal steroids — Anti-inflammatory sprays such as mometasone (Nasonex) and fluticasone (Flonase) reduce swelling of nasal membranes. Like antihistamines, nasal steroids can be most useful for those who have nasal allergies. Nasal steroids tend to produce less drying than antihistamines. Unlike nasal decongestants, nasal steroids can be used for prolonged periods.
Saline nasal sprays — These salt-water sprays are safe to use and can provide some relief by adding moisture to the nasal passages, thinning mucus secretions and helping to flush out any bacteria that may be present.
Pain relievers — Acetaminophen (Tylenol), ibuprofen (Advil, Motrin and others) or naproxen (Aleve) can be taken sinus pain.
Antibiotics — Your doctor may prescribe an antibiotic if he or she suspects that a bacterial infection is causing your sinusitis.
Not all cases of sinusitis require antibiotic treatment: Talk with your doctor about whether an antibiotic is right for you. Keep in mind that antibiotics can cause side effects, such as allergic reactions, rash and diarrhea. In addition, overusing antibiotics eventually leads to the spread of bacteria that no longer can be killed by the most commonly prescribed antibiotics.
When to call a professional
Contact a doctor if you experience facial pain along with a headache and fever, cold symptoms that last longer than seven to 10 days, or persistent green discharge from the nose. If your symptoms don't improve within a week of beginning treatment, call your doctor. Call sooner if symptoms are getting worse.
If you have repeated bouts of acute sinusitis, you may have allergies or another treatable cause of sinus congestion. Ask your doctor for advice.
Prognosis
The prognosis for acute sinusitis is very good. Most cases will go away within one to two weeks, often without antibiotics.
Additional info
National Institute of Allergy and Infectious Diseases (NIAID)
https://www.niaid.nih.gov/
American Academy of Allergy, Asthma, and Immunology (AAAAI)
https://www.aaaai.org/
About the Reviewer

Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.












