Bile duct diseases
- Reviewed by Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
What is a bile duct disease?
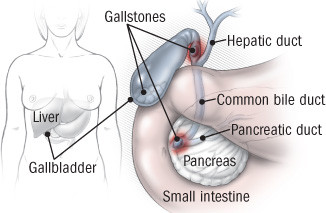
Your gallbladder stores bile until you eat, then releases bile into your small intestine to help digest food. Bile is made in the liver. It contains a mix of products such as bilirubin, cholesterol, and bile acids and salts. Bile ducts are drainage "pipes" that carry bile from the liver to the gallbladder and from the gallbladder to the small intestine.
A variety of diseases can affect your bile ducts. All impede the normal flow through bile ducts in some way, which is why the various diseases tend to cause similar symptoms.
Gallstones are the most common cause of blocked bile ducts. Stones typically form inside the gallbladder and can block the common bile duct, the drainpipe at the base of the liver. If the duct remains blocked, bilirubin backs up and enters the bloodstream. If bacteria accumulate above the blockage and back up into the liver, it may cause a severe infection called ascending cholangitis. If a gallstone stops in between the gallbladder and the common bile duct, an infection called cholecystitis may occur.
|
|
Less common causes of blockages include cancer of the bile duct (cholangiocarcinoma) and strictures (scars that narrow the ducts after infection, surgery, or inflammation).
Other bile duct diseases are uncommon, and include primary sclerosing cholangitis and primary biliary cholangitis (formerly called primary biliary cirrhosis). Typically diagnosed in mid-adulthood, these conditions create ongoing inflammation in the bile duct walls, which can narrow and scar the walls. Primary sclerosing cholangitis is more common in people with inflammatory bowel disease (ulcerative colitis or Crohn's disease). Primary biliary cholangitis is more common in women. It is sometimes associated with autoimmune diseases such as Sjögren's syndrome, thyroiditis, scleroderma, or rheumatoid arthritis.
Biliary atresia is a rare form of bile duct blockage that occurs in some infants two weeks to six weeks after birth, a time when the bile ducts have not completed their development normally.
The chronic conditions of primary sclerosing cholangitis, primary biliary cholangitis, and biliary atresia can result in inflammation and scarring of the liver, a condition known as cirrhosis.
Symptoms of a bile duct disease
Symptoms of a blocked bile duct may be abrupt and severe (for example, when a gallstone blocks the whole drainage system all at once), or they may appear slowly many years after bile duct inflammation started. Bile duct diseases often cause symptoms related to liver products backing up and leaking into the bloodstream. Other symptoms result from the bile ducts' failure to deliver certain digestive juices (bile salts) to the intestines, preventing the absorption of some fats and vitamins. Symptoms of a blocked bile duct include
- yellowing of the skin (jaundice) or eyes (icterus), from the buildup of a waste product called bilirubin
- itching (not limited to one area; may be worse at night or in warm weather)
- light brown urine
- fatigue
- weight loss
- fever or night sweats
- abdominal pain, especially common on the right side under the rib cage
- greasy or clay-colored stools
- diminished appetite.
Diagnosing a bile duct disease
Your doctor may suspect that you have a bile duct problem if you have any of the classic symptoms or if a blood test shows that you have a high level of bilirubin. Your doctor will take your medical history and examine you to look for clues that could explain damage to the bile ducts and liver. Because liver inflammation (hepatitis) and liver scarring (cirrhosis) can cause similar symptoms, your doctor will ask about your alcohol use, drug use, and sexual practices, all of which can result in liver disease.
If you have gallstones, have had pancreatitis or abdominal surgery, or have symptoms of an autoimmune condition (such as arthritis pain, dry mouth or eyes, skin rashes, or bloody diarrhea), tell your doctor. Because some medicines can slow drainage through the bile ducts, your medicines should be reviewed.
You will need blood tests to measure your levels of alkaline phosphatase, bilirubin, and/or gamma-glutamyl transferase (GGT). These are markers of bile duct obstruction. Other blood tests may suggest liver inflammation or cirrhosis. Occasionally, specialized blood tests may be helpful, such as antibody tests to diagnose primary biliary cholangitis or primary sclerosing cholangitis. A blood test with a high level of CA 19-9 may suggest a diagnosis of cholangiocarcinoma.
If your doctor suspects a bile duct problem, additional tests will depend on the suspected cause of the disease. Commonly used tests include:
- Right upper quadrant ultrasound. This provides pictures of the liver, gallbladder, and common bile duct. For example, it can show enlargement of the ducts above a blockage.
- Computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of the liver.
- Endoscopic retrograde cholangiopancreatography (ERCP), an examination in which a small camera on a flexible cord is inserted through your mouth and down past your stomach to the opening where the common bile duct empties into your stomach. A dye can be injected into the common bile duct that will appear on x-rays. How the bile ducts look on the x-rays can provide clues to the problem. Sample cells from the bile duct walls can be examined under a microscope for evidence of cancer. Treatments to relieve blockages can be performed during this examination.
- Magnetic resonance cholangiopancreatography, an examination similar to the endoscopic exam above. The advantage: MRI images can be obtained without passing an endoscope into the stomach. The disadvantage of this test is that tissue for a biopsy (laboratory examination) cannot be obtained.
- Cholangiography (x-rays of the bile ducts), which can also be done after dye is injected into the liver. This enables doctors to watch the flow of bile as it drains from the liver. Tissue for biopsy can be obtained during this procedure, and any blockages or narrowing can be relieved.
- A liver biopsy sample, obtained using a needle through the skin. The tissue is examined for evidence of inflammation or cancer.
If you have a chronic form of bile duct disease, your doctor may check you for cholesterol abnormalities or osteoporosis. Both of these conditions are more common in someone with longstanding bile duct drainage abnormalities.
Expected duration of a bile duct disease
To treat a gallstone blockage and infection (cholecystitis), doctors first prescribe antibiotics. After the infection subsides, a surgeon removes the gallbladder.
Symptoms caused by a scar (stricture) may improve rapidly after treatment restores the duct's drainage.
Symptoms of primary biliary cholangitis and primary sclerosing cholangitis are long-lasting diseases. They may steadily get worse and lead to cirrhosis and liver failure after years of damage. When liver failure develops, a liver transplant can improve survival. However, primary sclerosing cholangitis and primary biliary cirrhosis can return after transplant.
Preventing a bile duct disease
If you are overweight or have high cholesterol, you are at higher risk of developing gallstones. To avoid trouble, work toward a healthy weight through diet and exercise. Also, a near-starvation diet aimed at rapid weight loss can also result in gallstone formation.
Although cholangiocarcinoma is uncommon, smoking appears to increase the risk.
Certain parasite infections (Clonorchis sinensis and Opisthorchis viverrini, also known as Chinese liver fluke) are associated with a higher risk of bile duct diseases. If you travel to Southeast Asia, eat fish only if it is well cooked. If you do eat undercooked fish while traveling in this area, ask your doctor for a stool parasite test, especially if you have symptoms of weight loss or diarrhea.
Treating a bile duct disease
To treat a gallstone blockage accompanied by signs of persistent pain or infection, a gastroenterologist or surgeon can remove stones in the bile duct using endoscopic retrograde cholangiopancreatography (ERCP). The endoscope cuts through the base of the common bile duct, allowing a stone to pass through. In some cases the endoscopist may insert various devices into the bile duct to extract the stone. This same procedure can widen an area of scarred bile duct (a stricture) by inserting and expanding a wire coil (called a stent) within the duct. Doctors generally recommend that anyone with a persistent or recurrent bile duct blockage from a gallstone have his or her gallbladder removed.
Ascending cholangitis caused by a bacterial infection requires hospitalization and intensive intravenous antibiotic therapy. If there is any blockage in the common bile duct, it needs to be cleared promptly by ERCP or other surgical procedure.
It's rare to find bile duct cancer early, but if it is found early, it can be treated with surgery. When cancer is more advanced, surgery cannot totally remove the tumor. Surgical procedures can help cancer patients feel better, even if they cannot provide a cure. Surgery can reroute the bile duct to allow better drainage. Radiation treatments can help to shrink, but not cure, a bile duct tumor.
Biliary atresia, the failure to develop normal bile ducts in infants, can be treated by surgery. One method uses a portion of the baby's intestines to substitute for missing segments of the bile duct. Another method requires rerouting the bile drainage and additional intestinal surgery. However, most babies with this condition continue to have inflammation due to poor drainage, and eventually develop scarring (cirrhosis) and require a liver transplant.
Because both primary biliary cholangitis and primary sclerosing cholangitis can cause severe liver failure, a liver transplant may be needed for long-term survival. Treatment may reduce symptoms or delay the progression of the disease. In primary biliary cholangitis, the medicine used most often is ursodiol (Actigall).
The most bothersome symptom in chronic bile duct disease, itching, can be reduced with medicine — cholestyramine (Questran) or colestipol (Colestid) — that prevents irritants in the gut from being absorbed. Another medicine, naloxone, might neutralize irritants that cause itching. If greasy stools are a problem, a low-fat diet may be helpful. Doctors recommend multivitamin supplements to improve nutrition.
When to call a professional
If you develop yellowing of the skin or eyes, contact your doctor. If you also have fever or abdominal pain, call for professional advice immediately.
Prognosis
Infections related to gallstone blockage have excellent results when treated. Even the most severe infection, ascending cholangitis, has a low death rate if treated promptly.
The prognosis for primary sclerosing cholangitis and primary biliary cirrhosis has improved with better medical treatment and the potential for liver transplantation.
The prognosis for people with cholangiocarcinoma is better if the cancer is discovered while it is still confined to the duct. It can then be treated surgically. Once the cancer has spread, the survival rate is much lower.
Additional info
American Liver Foundation
https:/liverfoundation.org/
National Digestive Diseases Information Clearinghouse (NDDIC)
https://digestive.niddk.nih.gov/
American Gastroenterological Association
https://www.gastro.org/
American College of Gastroenterology (ACG)
https://gi.org/
About the Reviewer

Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.