Gastroesophageal reflux disease (GERD)
- Reviewed by Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
What is it?
Gastroesophageal reflux disease (GERD) is commonly called heartburn. This digestive disorder most often causes a burning and sometimes squeezing sensation in the mid-chest.
In GERD, acid and digestive enzymes from the stomach flow backward into the esophagus, the tube that carries food from your mouth to your stomach. This backward flow of stomach juices is called "reflux." These caustic stomach juices inflame the lining of the esophagus. If GERD is not treated, it can permanently damage the esophagus.
A muscular ring seals the esophagus from the stomach. This ring is called the esophageal sphincter. Normally, the sphincter opens when you swallow, allowing food into your stomach. The rest of the time, it squeezes tight to prevent food and acid in the stomach from backing up into the esophagus.
In most people with GERD, however, the esophageal sphincter does not seal tightly. It remains relaxed between swallows. This allows digestive juices to enter the esophagus and irritate the esophageal lining.
Many things can weaken or loosen the lower esophageal sphincter. These include
- certain foods
- smoking
- alcohol
- pregnancy
- many medications
- increased abdominal pressure, because of obesity or pregnancy
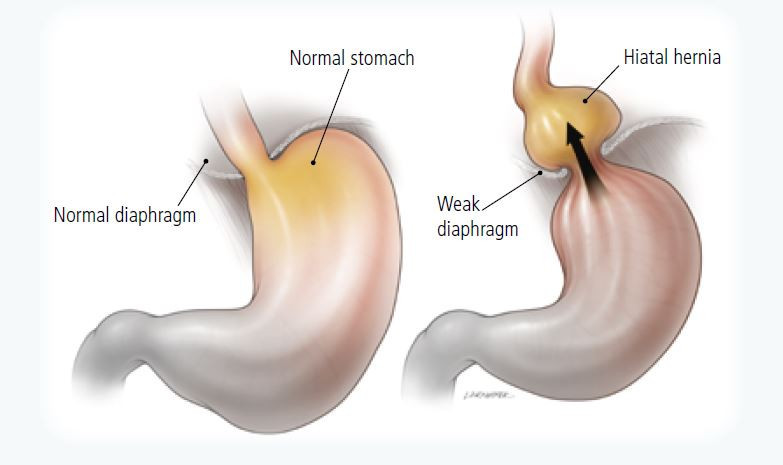
- a bulge in the stomach (hiatal hernia) that protrudes above the diaphragm.
|
|
Prolonged exposure to acid can cause the esophagus to
- become inflamed
- narrow
- develop an open sore.
|
|
Long-term exposure to acid also can lead to a condition called Barrett's esophagus. Barrett's esophagus increases the risk of esophageal cancer.
For many people with GERD, heartburn is not merely an occasional discomfort. Rather, it is a frequent, even daily, ordeal.
Symptoms
Symptoms of GERD may include
- sharp or burning chest pain behind the breastbone. This is also known as heartburn. It is the most common symptom of GERD. Heartburn may be worse when you eat, bend over, or lie down.
- tightness in your chest or upper abdomen. The pain may wake you up in the middle of the night.
- regurgitation, the backflow of stomach fluids into your mouth
- nausea
- a recurring sour or bitter taste in the mouth
- difficulty swallowing
- hoarseness, especially in the morning
- sore throat
- coughing, wheezing, or repeatedly needing to clear your throat.
Diagnosis
Your doctor will ask you:
- how often you have heartburn or other symptoms of GERD
- whether your symptoms are worse when you lie down or bend over
- whether your symptoms are relieved by over-the-counter heartburn remedies.
Your doctor also will review your current medications. Some medications can loosen the esophageal sphincter. These include
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen
- blood pressure or heart medications, such as calcium-channel blockers and nitroglycerin
- osteoporosis drugs called bisphosphonates
- progestins, such as progesterone
- medicines that reduce the amount of saliva you produce, such as antihistamines and antidepressants.
Pain that feels like heartburn also can be a symptom of coronary artery disease. Your doctor may ask whether you have any symptoms of heart problems. He or she may test for heart problems.
If your only complaint is mild heartburn and your physical examination is normal, your doctor may suggest lifestyle changes and over-the-counter medications. You may not need any special diagnostic testing or prescription treatment.
If you have more serious symptoms, or if your heartburn is not relieved by medications, you will need further testing. Serious symptoms include severe, long-lasting heartburn, difficulty swallowing, or weight loss.
The best test for GERD is an endoscopy. The doctor looks directly at your esophagus with an endoscope. This is a flexible tube that can be passed through the mouth and throat. Endoscopy usually is done by a gastroenterology specialist.
During endoscopy, your doctor may take a small sample of tissue to be examined in a laboratory. Your doctor also may look at your stomach and first part of the small intestines with the endoscope.
You also may have one or more of the following tests:
- Barium swallow — an x-ray test that outlines the esophagus.
- Cardiac evaluation — to check for heart disease.
- Esophageal manometry or motility studies — to check the squeezing motion of your esophagus when you are swallowing.
- Esophageal pH monitoring — uses electrodes to measure the pH (acid level) in the esophagus. It is usually done over a 24-hour period.
Expected duration
Without treatment, GERD is typically a long-term problem.
Symptoms may be relieved within days of treatment. But for many patients, several weeks of treatment are needed before symptoms lessen or resolve.
Treatment often has to continue for a long period. Even with daily medication, many people with reflux continue to have symptoms.
Prevention
There are a lot of things you can do to prevent the symptoms of GERD. Some simple lifestyle changes include:
- Elevate the head of your bed at least 6 inches. If possible, put wooden blocks under the legs at the head of the bed. Or, use a solid foam wedge under the head portion of the mattress. Simply using extra pillows may not help. Lying on your left side also can help reduce acid reflux.
- Avoid foods that cause the esophageal sphincter to relax during their digestion. These include
- coffee
- chocolate
- fatty foods
- whole milk
- peppermint
- spearmint.
- Limit acidic foods that make the irritation worse when they are regurgitated. These include citrus fruits and tomatoes.
- Avoid carbonated beverages. Burps of gas force the esophageal sphincter to open and can promote reflux.
- Eat smaller, more frequent meals.
- Do not lie down after eating.
- Do not eat during the three to four hours before you go to bed.
- If you smoke, quit.
- Avoid drinking alcohol. It loosens the esophageal sphincter.
- Lose weight if you are obese. Obesity can make it harder for the esophageal sphincter to stay closed.
- Avoid wearing tight-fitting garments. Increased pressure on the abdomen can open the esophageal sphincter.
- Use lozenges or gum to keep producing saliva.
Treatment
Treatment for most people with GERD includes lifestyle changes as described above and medication. If symptoms persist, surgery or endoscopy treatments are other options.
Medications
There are several medications that can be used to treat GERD. They include:
- Over-the-counter acid buffers — Buffers neutralize acid. They include Mylanta, Maalox, Tums, Rolaids, and Gaviscon. The liquid forms of these medications work faster, but the tablets may be more convenient.
Antacids that contain magnesium can cause diarrhea. And antacids that contain aluminum can cause constipation. Your doctor may advise you to alternate antacids to avoid these problems. These medicines work for a short time and they do not heal the inflammation of the esophagus.
- Over-the-counter H2 blockers — These drugs cause the stomach to make less acid. They are effective in patients with mild to moderate symptoms. They include famotidine (Pepcid AC), cimetidine (Tagamet HB), and nizatidine (Axid).
- Over-the-counter proton-pump inhibitors (PPIs) — PPIs shut off the stomach's acid production.
PPIs are very effective. They can be especially helpful in patients who do not respond to H2 blockers and antacids. These drugs are more potent acid-blockers than are H2 blockers, but they take longer to begin their effect.
- Prescription medications — Prescription medications include:
- H2 blockers — These are prescribed at higher doses than those available in over-the-counter forms.
- Proton-pump inhibitors (PPIs)— A variety of PPIs are available by prescription.
- Motility drugs — These medications may help to decrease esophageal reflux. But they are not usually used as the only treatment for GERD. They help the stomach to empty faster, which decreases the amount of time during which reflux can occur.
- Mucosal protectors — These medications coat, soothe, and protect the irritated esophageal lining. One example is sucralfate (Carafate).
Surgery
Surgery is an option for people with severe, difficult-to-control GERD symptoms. It may also be considered for people who have complications such as asthma or pneumonia, or scar tissue in the esophagus. Some people who do not want to take medications for a long time may choose surgery.
Surgery for GERD can be done using camera-guided instruments. This technique is called laparoscopic surgery. Laparoscopic surgery requires smaller incisions than conventional surgery.
In a procedure called Nissen fundoplication, excess stomach tissue is folded around the esophagus and sewn in place. This holds extra pressure around the weakened esophageal sphincter.
This operation appears to relieve symptoms about as much as prescription acid-blocking medicines. The success rates of surgery might be lower for people whose symptoms are not relieved by anti-acid medicines. Following surgery, some people have a lasting bothersome side effect. But most people who undergo surgery are very satisfied with the results.
Potential side effects include swallowing difficulty, diarrhea, and the inability to belch or vomit to relieve bloating or nausea.
|
|
Endoscopy treatments
The lower esophageal sphincter can sometimes be tightened using an endoscope. The procedures currently used are stitching (plication) and radiofrequency heating (the Stretta procedure). These procedures are newer and long-term success still needs to be determined.
Prognosis
Most patients improve after treatment with medication. But it can take weeks of treatment before symptoms begin to improve.
Additional info
National Digestive Diseases Information Clearinghouse
https://digestive.niddk.nih.gov/
American College of Gastroenterology (ACG)
https://www.gi.org/
About the Reviewer

Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.