Cardiomyopathy: Symptoms, diagnosis and treatment
Any heart disease in which the heart muscle (myocardium) weakens can be known as cardiomyopathy. This broad term covers many conditions, all of which result in injury to the heart muscle and impaired heart function. Cardiomyopathy often leads to heart failure.
In some forms of cardiomyopathy, the weakened heart muscle becomes thinned; in other forms it becomes abnormally thickened. In both cases, the ventricles of the heart have trouble pumping blood as effectively as they should. Blood can stagnate in the heart, making it more likely to form clots. If a clot breaks free and enters the circulation, it can cause a stroke if it lodges in an artery that nourishes the brain, or a pulmonary embolism if it lodges in an artery to the lungs.
The beleaguered heart muscle can also become prone to potentially dangerous abnormal heart rhythms.
Cardiomyopathy can be caused by:
- myocarditis, an inflammation of the heart muscle, often due to a viral infection or a chronic inflammatory condition such as lupus.
- coronary artery disease, the accumulation of cholesterol-filled plaque in the arteries that nourish the heart. It can weaken the heart muscle by reducing blood flow to much of the heart.
- drinking too much alcohol (alcoholic cardiomyopathy) can result from a lifetime of binge drinking or the cumulative effects of daily heavy drinking.
- invasion of heart muscle by abnormal cells or other material (restrictive cardiomyopathy).
- an inherited condition called hypertrophic cardiomyopathy which causes a thickening of the heart muscle, especially the wall between the two ventricles. In severe cases, the extra muscle obstructs the passage of blood out of the heart and may cause fainting or even sudden death. This disease usually occurs before the age of 40 and can affect children as young as age 10. It has been responsible for the deaths of several young athletes.
Symptoms of cardiomyopathy
In its earlier stages, cardiomyopathy may cause no symptoms. It may be discovered by accident, for example when a chest x-ray performed to diagnose another condition shows an enlarged heart.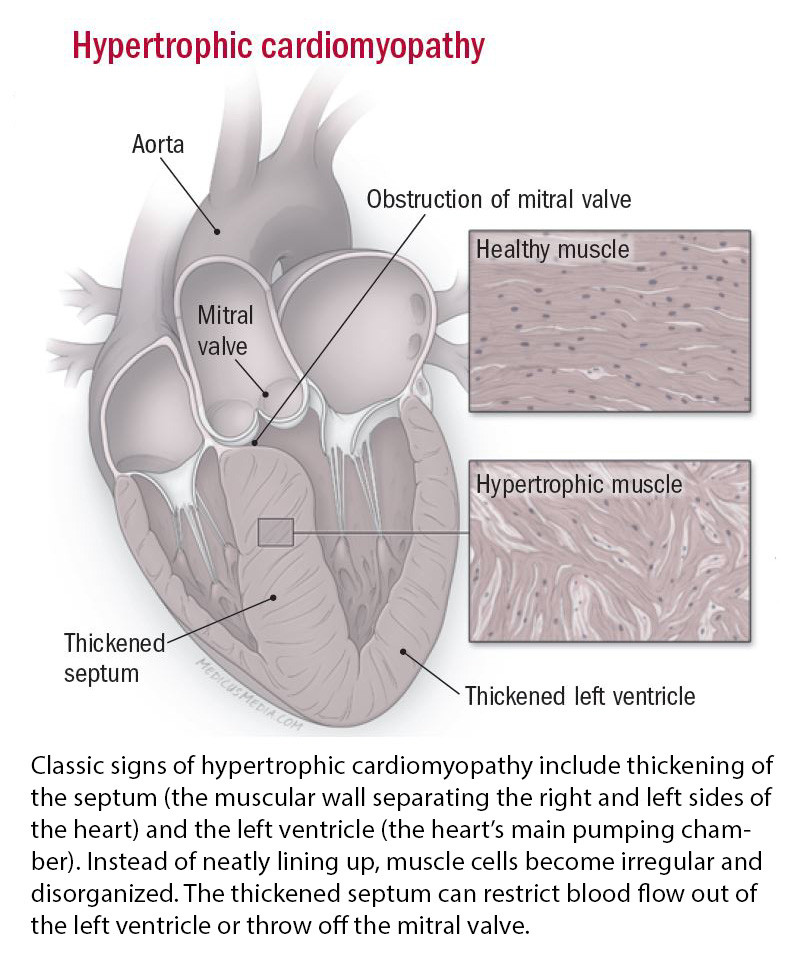
Common cardiomyopathy symptoms include:
- unexplained fatigue
- weakness
- breathlessness with even mild exertion or when lying down
- palpitations
- light-headedness
- fainting
- chest pain
Diagnosing cardiomyopathy
The diagnosis of cardiomyopathy is often clear from an individual's descriptions of his or her symptoms, the results of a physical examination, and the results of a chest x-ray, echocardiogram, and electrocardiogram.
Occasionally, a test called an endomyocardial biopsy is necessary. In this test, a catheter is inserted into a vein in the neck and passed down into the heart. A small piece of the inner heart wall is removed using a tiny metal device at the tip of the catheter. The sample of heart tissue is then examined under the microscope.
Treating cardiomyopathy
There are treatments for all forms of cardiomyopathy, including the two most common causes of symptoms: heart failure and abnormal heart rhythms.
People who have alcoholic cardiomyopathy seem to be particularly sensitive to the effects of alcohol; giving up drinking alcohol is the most important step in treating the condition. After that, the symptoms of heart failure can be controlled with drugs and dietary changes.
Treating hypertrophic cardiomyopathy can help control symptoms of chest pain and shortness of breath. More importantly, it can decrease the risk for sudden cardiac death. Usually this requires taking a beta blocker or calcium channel blocker. A medication to prevent abnormal heart rhythms may also be needed. It's also important to avoid strenuous exercise because it can trigger an abnormal heart rhythm that can cause sudden cardiac death.
Some individuals with cardiomyopathy benefit from the placement of a pacemaker or implantable cardioverter-defibrillator to maintain a steady heart rhythm.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.















