When the lights suddenly go out
Why fainting happens, and how to nip it in the bud.
Faint, black out, swoon, pass out. They're all names for the same thing — a temporary loss of consciousness followed by a fairly rapid and complete recovery. It's frightening when it comes out of the blue, more so when it happens again and again. The technical term, syncope (SIN-kuh-pee), comes from a Greek word that means to cut short or interrupt. What's being interrupted is blood flow to the brain.
Key points
|
Going, going, gone
It is harder for the heart to pump blood up to the brain than down to the toes. Blood pressure helps overcome the downward tug of gravity and push blood to the head.
We tend to think of blood pressure as a relatively stable entity. It isn't. It changes every time you stand up, sit down, bend over, eat, sneeze, go to the bathroom, get stressed, relax, or heft a bag of groceries. The human body is designed to counter these shifts and quickly bring blood pressure back to its usual point. This requires an intricate feedback system that involves sensors in the aorta and in the carotid arteries leading to the brain. These sensors stimulate a host of nerve and hormone signals that change how fast the heart beats, how much blood it pumps with each beat, and the contraction and relaxation of blood vessels. But some diseases, some drugs, and sometimes even aging interfere with these near-instantaneous corrections, causing temporary drops in blood flow to the brain.
Unlike most tissues, the brain doesn't store energy. Instead, it requires a constant supply of sugar and oxygen. Halting blood flow for just three to five seconds is enough to put the brain into an energy-conserving shutdown. The brain's signals to nerves and muscles stop, and the person slumps to the ground. Once the body is horizontal, it's easier for the heart to pump blood to the head, and the brain "wakes up" again.
Many things can cause sudden low flow to the brain that leads to fainting. The causes can be grouped loosely into two camps: problems outside the heart (noncardiac syncope), which account for the majority of faints, and problems in the heart (cardiac syncope).
Getting to the heart of a faintFiguring out what caused a fainting spell is the best way to prevent it from happening in the future. The most important piece of evidence is your story of what happened, especially if it can be corroborated by an eyewitness or two. Your description can suggest a vasovagal reaction (fainting due to standing too long in the heat, getting a shot, etc.), orthostatic hypotension (fainting when you stand up), or something more serious. A physical exam is in order no matter how straightforward the story. An electrocardiogram (ECG) and echocardiogram are essential tests for evaluating anyone who has fainted. The echocardiogram can spot hidden problems in the left ventricle or other forms of structural heart disease that can cause fainting. The ECG can detect irregularities in the heart's rhythm that could be the culprit. Unfortunately, capturing erratic heartbeats in the act is like finding the proverbial needle in a haystack. If you have fainted a few times for no apparent reason, and the ECG was "fine," your doctor might ask you to wear a device called a Holter monitor that continuously records the heart's electrical patterns for a 24-hour period. Longer-term monitoring can be done with a wearable loop recorder or an implanted recorder. These devices constantly monitor the heartbeat but store only the last several minutes. When a fainting spell hits, you press a button to freeze the information in the recorder. Another diagnostic test is the tilt test, in which your blood pressure and heart rate are measured while lying flat on a moveable table, and then again when the table is tilted so you are almost, but not quite, standing upright. |
Noncardiac causes
The most common reason for fainting arises from crossed wires between the brain and the part of the nervous system (the vagus nerve) that regulates blood pressure and heart rate. In response to some trigger, the blood vessels in your legs relax, making it difficult for blood to return to the heart. Blood begins pooling in the legs. To make matters worse, the heart slows down just when it ought to be speeding up. Blood pressure drops, and so do you. Triggers can range from fear, pain, or intense emotional stress to having blood drawn or standing for too long. Less common triggers include sneezing, going to the bathroom, lifting weights, a shirt collar rubbing against the side of the neck, and even playing a brass instrument.
Some people have faint-inducing drops in blood pressure when they get out of bed or stand up from a chair (called postural or orthostatic hypotension) or after eating (called postprandial hypotension). To understand postural hypotension, imagine your body as a tube of fluid. When you lie down, the fluid distributes itself fairly evenly from head to toe. When you stand up, gravity pulls blood downward. Up to a quart of blood pools in the legs (that's about one-fifth the total in the average adult), reducing the amount that is returned to the heart. The next few heartbeats deliver less blood than usual, so blood pressure plummets. Standing after sitting has much the same effect. Dehydration can contribute to orthostatic hypotension, or sometimes even cause it. A similar thing happens after eating. As the body directs extra blood toward the stomach and intestines to aid digestion, less is available to the heart, causing blood pressure to fall.
Cardiac syncope
Fainting caused by trouble in the heart is more worrisome than noncardiac syncope. Rhythm problems are the most common culprit here. The heart may beat too slowly (bradycardia) because of a defect in its electrical system or the influence of medications. It can also beat too fast (tachycardia) because of a rhythm disorder such as atrial fibrillation or ventricular tachycardia. The latter is especially dangerous, since it can turn into ventricular fibrillation, the most common cause of sudden cardiac arrest.
Anything that obstructs blood flow through the heart can also lead to fainting. It could be a blocked or severely narrowed heart valve, a large blood clot, or even a tumor in the heart. Other cardiac causes of fainting include a severely enlarged heart (hypertrophic cardiomyopathy), a tear in the aorta, heart attack, or damage to the heart muscle.
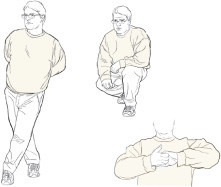
Squeezing away a faint
If you feel lightheaded or feel like you might faint, try crossing your legs and tensing the muscles in the lower body, squatting and tensing, or contracting the muscles in your arms by clasping your hands and pulling. Each of these maneuvers can boost blood pressure. It might be enough to stop the faint in its tracks, or it might just give you time to lie down or move to a safe place. Illustrations by Rob Flewell, with permission from the Journal of the American College of Cardiology. |
Fighting a faint
Most people get a few seconds of warning that a vasovagal faint is on its way. They turn pale, become dizzy or lightheaded, and may feel nauseous or break out in a cold, clammy sweat. This early warning is sometimes enough time to nip a faint in the bud. Sitting or lying down often works, as does the proverbial "sit down and put your head between your knees." Tensing the muscles in your hands, arms, and legs (see "Squeezing away a faint") can also help those who are composed enough to remember these maneuvers.
It may also be possible to train your body to fight faints. Writing in the May 12, 2009, Journal of the American College of Cardiology, Drs. David G. Benditt and John T. Nguyen of the University of Minnesota Medical School describe an exercise called tilt training. It involves standing with your back against a wall while your heels are about six inches from the wall (see "Tilt training").
If you know you will be in a situation in which you might faint — say you tend to pass out at the sight of blood but your daughter wants you to be with her when she gives birth to your first grandchild — here are a few things to do beforehand:
-
Drink a quart of juice and eat a bag of potato chips. The idea is to load up with fluid, so there is no chance of dehydration.
-
Get some special stockings that put pressure on the calf and thigh muscles. This will help to prevent pooling of blood in the legs.
-
Have a reclining chair in the room, preferably one in which the legs can be raised to the level of the heart if light-headedness occurs.
Tilt training
Some people can teach their bodies to overcome neurally mediated syncope, caused by crossed signals between the brain and the nervous system. Stand with your back lightly against a wall while your heels are about six inches (15 centimeters) from the base of the wall. Do this for three to five minutes without moving, twice a day. Every few days, add a minute or so to the standing time until you can do 20- to 30-minute sessions without feeling faint. After that, try to do 20 minutes of wall standing three to four times a week. It's best to do this in a carpeted room, and to have someone with you in case you faint. |
Don't take it lying down
Most of the time, fainting is a harmless — though disconcerting — event. Sometimes, though, especially in older people, it can be a warning sign of a potentially dangerous heart problem. For that reason, always let your doctor know if you've fainted, even if you think it was nothing to worry about. It's better to be reassured it was "just a vasovagal spell" than to overlook something that could cause a more serious problem down the road.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.