Exercise stress test
The treadmill test can reveal hidden problems in the heart.
One way to judge the health of the heart and the arteries that supply it with oxygen and nutrients is to make them work harder. That's the principle behind one of the most commonly used tests in cardiology, the exercise stress test (also known as the exercise tolerance test, treadmill test, or just the stress test). It's much the same thing a mechanic does when he or she races a car's engine.
Why it is done
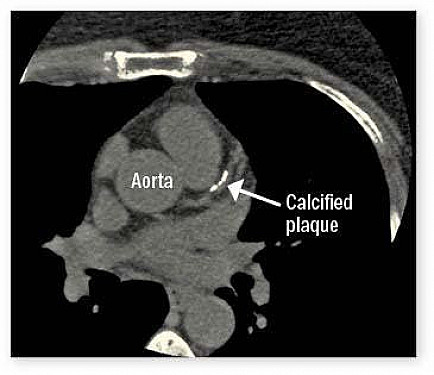
Exercise stress tests are done for a variety of reasons. The most common one is to detect a narrowing or blockage in one or more coronary arteries. This network of blood vessels supplies the heart muscle with oxygen and nutrients. When the heart is at rest, even an artery that is almost completely blocked may have enough blood flow to meet the needs of the section of heart muscle it supplies. But make the heart work harder, and the clogged vessel may not be able to handle the extra rush of blood needed by the hard-working muscle. This mismatch in demand and supply can cause angina — pressure or pain in the chest, jaw, left arm, or elsewhere that comes on with exercise or other stress and disappears with rest.
An exercise stress test can document low blood flow (ischemia) in the coronary arteries. It should be part of the work-up for anyone having angina or who might be a candidate for artery-opening angioplasty. Stress tests are also used to reveal hidden rhythm problems, assess some valves, gauge the safety of an exercise program, and monitor the effectiveness of treatment.
Procedure
The tools used to see how your heart performs during exercise include an electrocardiograph (ECG), a blood pressure cuff, and a treadmill (see "Stress test setup").
Stress test setup
The procedure for taking an exercise stress test is relatively straightforward. As you walk on a treadmill at progressively faster speeds, an electro-cardiograph measures your heart rate and the electrical activity in your heart, and your blood pressure is recorded periodically. |
The doctor, nurse, or technician running the test sticks a number of adhesive pads to your chest, then attaches a plastic-coated wire to each pad. The wires feed into the ECG, which records the electrical activity in your heart and how fast it is beating. A blood pressure cuff is wrapped around your arm. The machines record what is happening in your heart and arteries, first as you sit quietly, and then as you stand quietly.
When the baseline recordings are complete, you start walking on the treadmill at a slow pace (under 2 miles an hour). Every few minutes, the speed and steepness of the treadmill increase, making you work harder. In the most widely used test, called the Bruce protocol, there are seven stages, each one lasting for three minutes. If you get to the last stage, you'll be walking at 5.5 mph up a 20% grade. The goal is to get your heart working up to at least 85% of its maximum capacity. You finish with a few minutes of slow walking to cool down, and then stand or sit quietly for another 15 minutes or so as your heart returns to its resting state.
Throughout all this, your heart rate and electrical activity are constantly monitored, your blood pressure is checked every few minutes, and the clinician keeps tabs on how you look and how you feel.
Hardly anyone makes it through all seven stages. People who are out of shape or who aren't used to exercising typically stop early because they become too tired or out of breath. Some stop because of chest pain or leg pain. Sometimes the clinician stops the test because of worrisome changes on the ECG or in blood pressure. If the test is stopped before you reach your target heart rate, the results may not tell you or your doctor much.
A modified version of the test is used for people who are frail or out of shape. Bicycles can be used for people who have trouble walking; arm-powered exercise machines are available for those who can't use their legs.
Preparing for the test
Getting ready for an exercise stress test is much like getting ready for a brisk walk or jog around the neighborhood. Wear loose, comfortable clothing and shoes suitable for walking or running. Don't eat, smoke, or drink beverages containing caffeine or alcohol for three hours before the test.
Your doctor may ask you to stop certain medications that can interfere with the heart's response to exercise, like a beta blocker or digoxin, a day or more before the test.
If you have diabetes, ask your doctor when and what you should eat before the test, to make sure your blood sugar stays in the right zone. You may be asked to check your blood sugar before the test, and then again soon afterward and once or twice when you get home.
What the test shows
Different bits of data collected during an exercise stress test can point to problems inside the heart.
ECG. Changes in the ECG are key signs that part of the heart muscle isn't getting as much oxygenated blood as it needs. This is often indicated by an elevation or depression in part of the ECG called the ST segment (see figure).
ST-segment depression
One worrisome change during exercise is a depression of the ST segment on the electrocardiogram. It is a tell-tale sign that part of the heart is not getting enough oxygen. |
Heart rate. Two possible indicators of ischemia or trouble in the heart's electrical system are if the heart fails to beat as fast as it should with strenuous exercise or it takes too long to slow down after exercise.
Blood pressure. When the cardiovascular system is healthy, systolic blood pressure (the pressure generated when the heart contracts) increases with exercise, and can easily reach 200. If it doesn't climb much above 120, or begins falling, it can indicate an overworked left ventricle or a valve or rhythm problem.
Rhythm changes. The appearance of nonstandard heart rhythms can suggest coronary artery disease, cardiomyopathy, or an inherited heart problem. The most ominous is ventricular tachycardia, an exceptionally rapid beating of the heart's lower chambers.
Recovery. In many people, the ECG shows brief alterations in the rhythm of the ventricles (the lower chambers of the heart) or the atria (the upper chambers) as the heart recovers after exercise. These erratic beats don't indicate ischemia, but they have been linked with later cardiac problems.
Special situations
For most people, a standard stress test is sufficient. Others need more precise information, and some cannot exercise. Variations and alternatives include:
Nuclear stress test. A radioactive tracer is injected into the bloodstream as you exercise to measure blood flow to the heart muscle.
Stress echocardiography. A clinician uses an ultrasound probe to record images of your heart before and after you exercise. These images can identify parts of the heart that aren't receiving enough blood.
Pharmacological stress test. Instead of exercise, a heart-stimulating drug such as dobutamine or adenosine is used to make the heart work harder.
What it means
An exercise stress test is a good — but not great — indicator of the health of the heart and coronary arteries. It works quite well for people who are likely to have cholesterol-clogged arteries and who can exercise long enough to reach their maximum heart rate. The test isn't as good for people at low risk of heart disease, or those who are too frail or out of shape to exercise long enough.
The exercise stress test should be used when some sort of heart disease is suspected. If you are feeling fine, don't have one to "check under the hood." Just as the test misses some cases of heart disease, about 15% of the time it gives misleading false-positive results. Those can lead to needless worry and further testing, often including an angiogram. Most experienced cardiologists can recall at least one patient who had a serious complication from an angiogram done in response to what turned out to be a false-positive stress test.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.