What is vasculitis?
Ask the doctor
 Q.
After undergoing a battery of different tests, my father has been diagnosed with what his doctor described as a rare form of vasculitis. What can you tell me about this disease?
Q.
After undergoing a battery of different tests, my father has been diagnosed with what his doctor described as a rare form of vasculitis. What can you tell me about this disease?
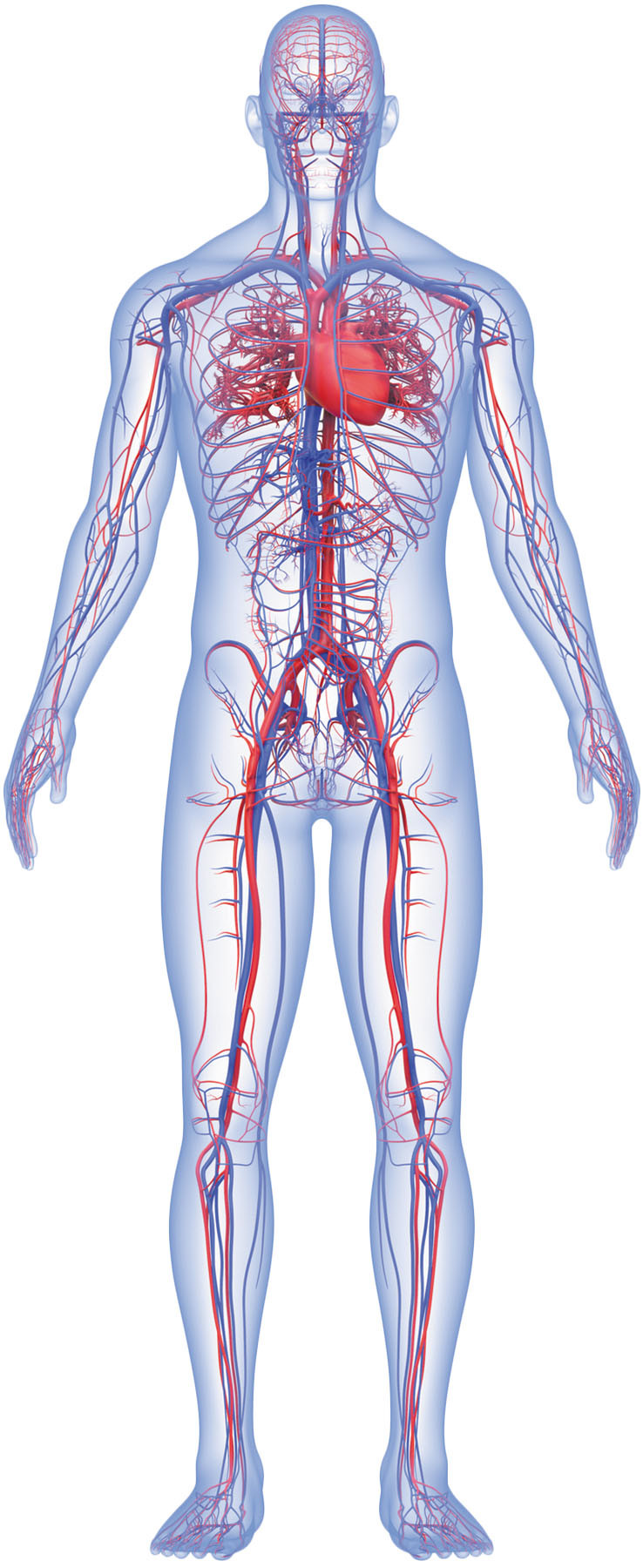
A. Vasculitis is an umbrella term for a group of nearly 20 rare conditions characterized by inflammation of the blood vessels, including the arteries, veins, and capillaries. The inflammation can cause damage that narrows, weakens, or scars large or small vessels that supply just one body part (such as the head) or many different organs.
The different types of vasculitis are classified by the size and location of the affected vessels. Symptoms can vary widely from person to person, which is one reason vasculitis can be difficult to diagnose. In fact, one recent study found that nearly three-quarters of people with vasculitis were initially misdiagnosed, most often with an infection or allergies.
Experts don't fully understand the cause of vasculitis, although many consider it an autoimmune disease, which happens when the immune system mistakenly attacks healthy tissue. Possible triggers for vasculitis include infections, allergies, or another autoimmune condition such as lupus, rheumatoid arthritis, or scleroderma.
Although vasculitis can occur at any age, some forms are more common after middle age. In people ages 50 and older, the most common is giant cell arteritis (also called temporal arteritis), which usually affects arteries in the neck and scalp, especially those just above the ears at the temples. Common symptoms include persistent, throbbing headaches and tenderness of the temples and scalp.
Another type, polyarteritis nodosa, tends to occur more in men than in women. It affects vessels in the skin, muscles, heart, kidneys, and intestines, causing symptoms such as purplish-blue blotches or ulcers on the skin and pain in the muscles, joints, and abdomen.
Tests to diagnose vasculitis may involve blood and urine tests, x-rays or other imaging tests, and in some cases, a small tissue sample (biopsy) taken from the affected organ. Milder forms of vasculitis, like those that affect just the skin, may resolve without treatment. But more serious cases require lifelong therapy, which starts by controlling inflammation (typically with steroids) to put the condition in remission. After that, immune-suppressing drugs can help prevent relapses. I always urge people diagnosed with vasculitis to seek care at medical centers with expertise in these unusual conditions. Most often, rheumatologists are the primary specialists who treat vasculitis, but other specialists may also be involved.
Image: © magicmine/Getty Images
About the Author

Deepak L. Bhatt, M.D., M.P.H, Former Editor in Chief, Harvard Heart Letter
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.