When incidental findings on scans reveal hidden heart disease
Imaging tests such as CT scans and mammograms can offer clues about the health of your heart's arteries.
- Reviewed by Christopher P. Cannon, MD, Editor in Chief, Harvard Heart Letter; Editorial Advisory Board Member, Harvard Health Publishing
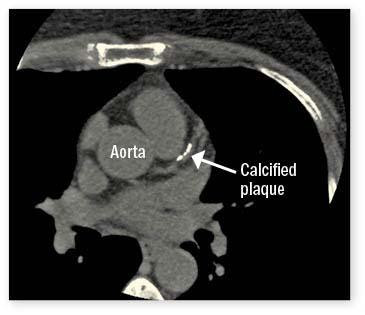
Liz, an artist living in North Carolina, had a CT scan several years ago to evaluate a torn muscle in her upper abdomen. The radiologist’s report included some additional concerning information: “Coronary arterial calcification much greater than expected for patient’s age.” Calcification is a marker for heart disease, since the fat-laden plaque that accumulates inside arteries often contains calcium, which is visible on CT scans. Liz, who was 56 at the time, consulted a cardiologist about the discovery. Four years later, she had bypass surgery to treat two severely narrowed coronary arteries.
When a medical test discovers something unrelated to the test’s original purpose, doctors call it an incidental finding. Cases like Liz’s are not unusual, especially since CT scans have become increasingly common in recent years. These scans take a series of rapid-fire x-rays which, when combined together, enable doctors to “see” structures inside the body.
Visualizing calcium deposits
A scan that focuses only on the heart, called a coronary artery calcium (CAC) scan, can detect and quantify calcium deposits in the heart’s arteries. These tests report a calcium score that ranges from 0 to 1,000 or higher. But they’re recommended mainly for people with an intermediate risk of heart disease, to help clarify treatment decisions.
“Calcium deposits can show up on diagnostic and screening CT scans as well as mammograms, so these tests can also provide a way to get more information about a person’s cardiovascular health,” says Dr. Rhanderson Cardoso, a cardiologist at Harvard-affiliated Brigham and Women’s Hospital. This so-called opportunistic screening may be especially valuable in people don’t have classic risk factors. Examples include people who don’t know their family medical history and those with an unrecognized genetic condition that causes very high cholesterol, he adds.
Chest CT scans
The prime source of incidental discoveries are chest CT scans, which people undergo for many reasons, says Dr. Cardoso. Common ones include assessing lung infections from pneumonia or COVID, checking for a blood clot in the lungs (pulmonary embolism), and screening for lung cancer (see “Lung and breast cancer screening recommendations”).
“Like many cardiologists, I routinely review my patient’s previous imaging studies, even if they’re not heart-related,” says Dr. Cardoso. These days, such reviews are often easier to do thanks to integrated electronic medical records used by large health care systems. Calcifications in chest CT scans are grouped into four categories: none, mild, moderate, or severe. That’s often enough for a cardiologist to make a solid decision about whether to maintain or intensify a person’s drug treatment to prevent heart disease progression, Dr. Cardoso says. If you’ve had a chest CT scan in the recent past, you can ask your physician or radiologist to re-check it for evidence of coronary calcifications if that information isn’t included in the original report.
Lung and breast cancer screening recommendationsCancer screening recommendations vary depending on your family history and other factors. For lung cancer, the American Cancer Society recommends yearly low-dose CT for people for current and former smokers ages 50 to 80 who have at least a 20-pack-year history of smoking. A pack-year is equal to smoking one pack (about 20 cigarettes) per day for a year. For women with an average risk of breast cancer, the American Cancer Society recommends annual mammograms from age 45 to age 54, and then every other year. The U.S. Preventive Services Task Force advises screening starting at age 50 and continuing every two years up to age 74. |
Mammograms
For women, mammograms may be another way to detect possible heart disease. These scans can pick up tiny specks of calcium in the arteries of the breast, which suggest there might also be calcifications in the heart. However, the connection between the two is not as robust, and findings on a mammogram are a less reliable predictor than those from a chest CT. Still, if your mammogram results mention breast arterial calcification, discuss the finding with your primary care physician. He or she should make sure your risk factors, such as blood pressure and cholesterol, are well controlled, Dr. Cardoso says. “If there’s any cause for concern, a CAC scan may be a good idea,” he adds.
Chest scan image courtesy of Ronald Blankstein, MD
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
About the Reviewer

Christopher P. Cannon, MD, Editor in Chief, Harvard Heart Letter; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
















