Carotid artery disease
The brain requires a constant supply of oxygen. Much of it comes from oxygen-rich blood delivered by the carotid arteries. These travel from the body's main artery, the aorta, up either side of the neck (where their pulses can be felt on either side of the trachea, or windpipe), and into the brain.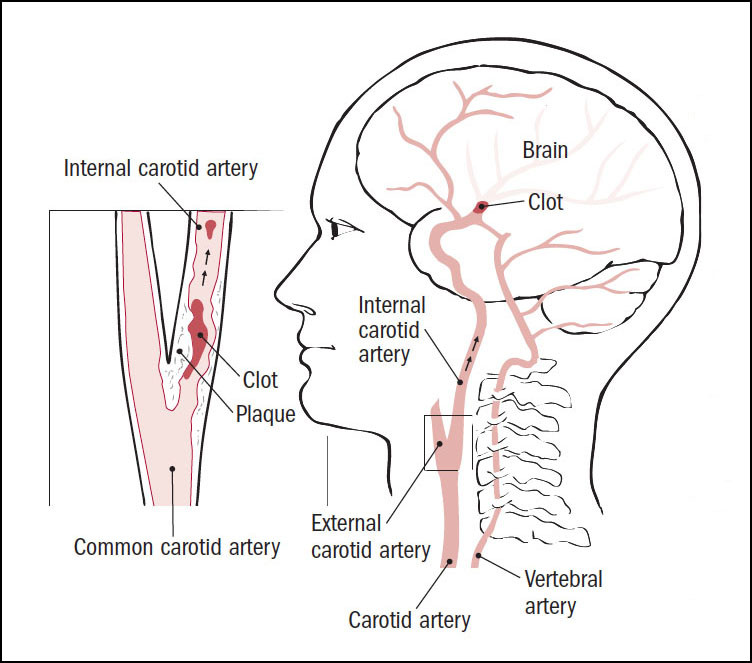
A cholesterol-laden plaque can narrow a carotid artery. This is called carotid artery disease.
A large plaque can slow blood flow to the brain. Even more worrisome is if a plaque breaks open. The blood clot that forms to seal the break can travel to the brain, causing a transient ischemic attack (mini-stroke) or stroke.
Symptoms of carotid artery disease
Carotid artery disease often causes no signs or symptoms until it severely narrows or blocks a carotid artery. Signs and symptoms may include a bruit (broo-EE), a transient ischemic attack, or a stroke.
Narrowing of a carotid artery produces turbulent blood flow. Like water rushing along a bubbling brook, turbulent flow in a blood vessel is noisy. Your doctor can hear that noise, called a bruit, by listening to your carotid arteries through a stethoscope. Unfortunately, many arteries with bruits have perfectly adequate blood flow, while some that are severely narrowed carry blood silently.
A transient ischemic attack, also known as a mini-stroke, may be the first sign of carotid artery disease. A mini-stroke is much like a full-blown stroke, except that the symptoms go away on their own within 24 hours.
The symptoms of transient ischemic attack include:
- sudden weakness or numbness in the face, arms, or legs, often on one side of the body
- trouble moving an arm or leg
- trouble speaking or understanding speech
- sudden trouble seeing in one or both eyes
- sudden dizziness or loss of balance
A mini-stroke is a warning sign that a stroke may be on the way. About 1 in 3 people who have mini-strokes later have strokes.
In some people, a stroke is the first symptom of carotid artery disease. The symptoms of a stroke are the same as those of a mini-stroke, but it can lead to long-term damage such as paralysis, vision or speech problems, and even death.
Diagnosing carotid artery disease
The starting point for detecting carotid artery disease is an ultrasound exam. It uses sound waves to create images of the carotid arteries. Carotid ultrasound is a good way to identify severe carotid narrowing, but it's less accurate for milder blockages.
Magnetic resonance angiography and computed tomography angiography can produce detailed images of carotid blockages. These scans create high-quality images of the carotid arteries. Computed tomography angiography involves radiation; magnetic resonance angiography does not.
Carotid angiography is an invasive test that requires inserting a thin tube called a catheter into a blood vessel in the arm or leg, and gently maneuvering it up to the carotid arteries. Once in place, the catheter injects a dye into the arteries. Movement of the dye through the carotid arteries is captured by a series of x-rays.
Treating carotid artery disease
Carotid artery disease can be treated with medication or with a procedure to remove the narrowing. In both cases, the goal is to prevent stroke.
Medical therapy involves taking medications to protect the arteries. These include:
- aspirin or other antiplatelet agent to prevent the formation of blood clots
- a cholesterol-lowering statin to treat artery-clogging atherosclerosis and stabilize cholesterol-filled plaques
- if needed, one or more medications to lower blood pressure
Two artery-opening options are available:
- carotid endarterectomy. In this operation, a surgeon opens the clogged carotid artery and removes cholesterol-filled plaque.
- angioplasty with stenting. In this procedure, a physician inserts a thin wire called a catheter into a blood vessel in the leg or neck and gently maneuvers it into the narrowed carotid artery. When the catheter is in place, a tiny balloon at its tip is expanded, flattening the plaque. The balloon expands a wire mesh cage called a stent and pushes it into the artery walls. This holds the artery open after the balloon and catheter are removed.
Medical therapy attacks atherosclerosis, the ultimate cause of carotid artery disease, throughout the carotid arteries and the rest of the body. A procedure treats only a single narrowing. In addition, carotid endarterectomy and angioplasty can both trigger strokes or cause other side effects, although the risk is low when done by an experienced clinician in a hospital that often does the procedure.
Two key factors can help make the right choice: the presence or absence of symptoms, and the degree of narrowing seen inside the carotid artery.
Individuals without symptoms
Individuals with carotid artery disease that is not causing any symptoms are best served, at least initially, by medical therapy, especially if the narrowing is less than 70%.
Individuals in whom carotid artery disease causes no symptoms but whose narrowing is greater than 70% can opt for medication or an artery-opening procedure.
Individuals with symptoms
Individuals with carotid artery disease who have had a transient ischemic attack or stroke should be considered for a procedure to open or clear a clogged carotid artery if the narrowing is greater than 50%. Those with severe narrowing (70% to 99%) stand to benefit the most, but patients with moderate narrowing (50% to 69%) may also gain some protection against future strokes.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.















