Sinusitis
How to get relief without antibiotics
More than 20 million Americans will have at least one bout of sinusitis this year. Most will be uncomfortable, and many will miss work or school. Nearly all will recover from their sinus infections, but an unfortunate few may develop complications. If you understand sinusitis, you can reduce your chances of developing the problem and if sinusitis strikes, you'll know how to speed your recovery and lower your risk of complications.
Your sinuses
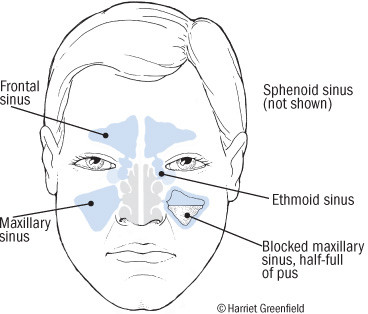
Your sinuses are air-filled chambers located in the bones of your face; because they surround the nose, they are also known as the "paranasal sinuses." Each of us has four pairs of sinuses (see figure).
Each of the sinuses is lined by a membrane that produces mucus. When you're healthy, the mucus is a thin, watery fluid that flows freely from your sinuses into the upper part of your nose. But when your sinuses become inflamed, the mucus gets thick and sticky, so it can't flow through the tiny openings, called ostia, that lead to the nose. Fluid builds up in the sinuses, causing pressure and pain, and just like that, you've got sinusitis.
Your sinuses
Your four pairs of sinuses are air-filled chambers located in the bones around your nose. The frontal sinuses are behind the forehead; the maxillary sinuses are behind the cheek bones; the ethmoid sinuses are behind the bridge of the nose; and the sphenoid sinuses are deeper in the skull behind the nose. |
What causes sinusitis?
Sinusitis is an infection most often caused by viruses or bacteria or both. Cold viruses and bacteria that get into our sinuses usually don't cause trouble unless sinus drainage is blocked. Blockage of the narrow sinus draining channels is the main reason we get sinusitis, and restoration of drainage is the key to treatment.
What triggers sinusitis?
The common cold is the leading culprit. The average adult gets two to three colds a year, and the average child gets six to 10. Colds are caused by viruses, not bacteria, and antibiotics are useless for treatment. But cold viruses produce swelling of the nasal tissues, which can sometimes block the sinuses. Colds also change the mucus, preventing it from doing its normal job of clearing viruses and bacteria from the sinuses.
You may get some sinus pressure when you get a cold, but that doesn't mean you have sinusitis or that you need an antibiotic. Only about one cold in 100 leads to sinusitis, and you can make the odds work for you by doing what it takes to keep your sinuses draining (see below). You can also help your cause by blowing your nose gently without pinching it tightly; forceful blowing can force bacteria up into your sinuses.
Many other things can block your sinuses and lead to infection. The list includes allergies, cigarette smoke and other irritating fumes, changes in barometric pressure during flying or scuba diving, nasal polyps, and a deviated nasal septum.
Sinus infection symptoms
Painful pressure is the main symptom of a sinus infection. Depending on which sinus is involved, the pain is in the forehead (frontal sinusitis), over the cheek or in the upper jaw and teeth (maxillary sinusitis), behind the eyes (ethmoid or sphenoid sinusitis), or at the top of the head (sphenoid sinusitis). Sinus pain usually increases when you bend forward.
Nasal congestion and a thick, dark-colored nasal discharge are also common during a sinus infection. When the mucus drips into your throat from the back of your nose, you'll notice a foul taste, and you may get bad breath or a cough. You may temporarily lose your sense of smell or taste. Finally, you may feel feverish, achy, and tired.
Sinusitis diagnosis
In most cases, your doctor can diagnose sinusitis simply by asking about your symptoms. If pressing over your sinuses causes pain, sinusitis is likely. CT scans can be very helpful if your sinusitis is unusually severe or if your doctor suspects complications; plain x-rays are less useful. ENT (ear, nose, and throat) specialists can also diagnose sinusitis by looking up your nose with a scope.
Sinus infection treatment: Promoting drainage
Many people with sinusitis will recover quickly and completely without taking antibiotics simply by promoting drainage. Here's what you should do:
- Drink lots of water. Good hydration helps keep the mucus thin and loose.
- Inhale steam. Linger in a hot shower. Boil a kettle, pour the water into a pan, and bend over the pan with a towel over your head to inhale the steam. Even hot tea or chicken soup will help; the secret ingredient is the steam. One way or another, inhale steam three to four times a day.
- Sleep with your head elevated. If your pain is only on one side, sleep with the pain-free side of your face on the pillow.
- Use decongestants. Tablets containing pseudoephedrine or phenylephrine are very helpful but may sometimes raise your blood pressure, speed your pulse, or make you jittery and keep you up at night. Nasal sprays containing phenylephrine or oxymetazoline don't have these side effects, but if you use them too often or for too long, your nose can become irritated or dependent on them.
- Ask your doctor about prescription nasal sprays containing steroids, particularly if you have allergies or if your sinusitis is stubborn.
- Use a saline (salt water) nasal spray to loosen mucus and rinse your sinuses.
- Use antihistamines wisely. They're great for allergies and when your nose waters from a cold, but they make mucus thick and hard to drain, the last thing you want in sinusitis.
- A warm compress on your face may soothe sinus pain. Over-the-counter pain relievers such as aspirin or acetaminophen will help reduce pain and fever.
Antibiotics for a severe sinus infection
You may be surprised that antibiotics are not listed as the first step in treatment. While many patients with sinusitis expect antibiotics, they aren't usually needed if good drainage is achieved.
Antibiotics have potential disadvantages. They can trigger allergic reactions or cause side effects. Widespread use of antibiotics has encouraged the spread of antibiotic-resistant bacteria ("superbugs"). And many of these drugs are expensive.
Still, if your sinusitis does not improve with two to four days of drainage therapy, or if it's very severe to begin with, it probably needs an antibiotic to help get rid of the trapped bacteria. Antibiotic therapy for just three to seven days is generally as effective as traditional 10- to 14-day treatment for uncomplicated acute sinusitis.
Many bacteria can cause acute sinusitis; the most common include some with fearsome names like Pneumococcus, Streptococcus, Hemophilus, and Moraxella. Unless you have a sinus puncture (an invasive test that's rarely performed by ENT specialists unless unusual organisms or complications are suspected), there's really no way to know which bacteria are causing your sinusitis. Cultures of your mucus or your nose, even if they are obtained through a nasal speculum, are not helpful because they are always contaminated by the many bacteria that live in every nose.
With these considerations in mind, many infectious disease specialists recommend initial sinusitis treatment with one of the old standbys, such as trimethoprim-sulfamethoxazole (a combination that includes a sulfa drug), amoxicillin (a type of penicillin), or doxycycline (a type of tetracycline). If these fail "" or if the patient is unusually ill to begin with "" doctors may turn to amoxicillin-clavulanic acid or a quinolone (such as levofloxacin).
Complications
The sinuses are surrounded by critical structures, including the brain, the eyes, and the skull. On rare occasions, sinus infections can spread to one of these areas. Notify your doctor promptly if your sinusitis gets worse with one or more of these warning symptoms:
- high fever
- severe headache
- mental confusion or stiff neck
- swelling of the cheek, forehead, or roof of the mouth
- a swollen, red, painful eye
- impaired vision
- difficulty breathing, swallowing, or speaking.
Fortunately, none of these problems is likely. Still, they serve to remind us that sinusitis is not just the sniffles. Patients with weakened immune systems always require careful medical evaluation and treatment for sinusitis.
Chronic sinusitis
Sinusitis that lasts more than three weeks or recurs more than three times a year is called chronic sinusitis. The most common cause of chronic sinusitis is inadequately treated acute sinusitis, and since the diagnosis and treatment of acute sinusitis have improved so much, chronic sinusitis is less common than it used to be.
Most patients with chronic sinusitis will benefit from an ENT evaluation, which usually includes looking inside both nostrils with a scope. The doctor may also order a CT scan. That's because anatomic problems such as nasal polyps or a deviated septum are often responsible. Since allergies are also present in many cases, you may want to pursue formal allergy testing.
Persistent nasal discharge and congestion are the main symptoms of chronic sinusitis. Unless flares of acute sinusitis develop, headache and fever are minimal.
In addition to the bacteria that cause acute sinusitis, Staphylococcus, anaerobic bacteria, and fungi may lead to chronic sinusitis. Antibiotics can be helpful, especially for flares, but they are less important than nasal irrigation, decongestants, and prescription nasal spray. If allergies are present, antihistamines can help. In severe cases, oral steroids may be necessary. As with acute sinusitis, the key to successful treatment is drainage. In the case of chronic sinusitis, though, surgery may be needed. Your ENT doctor may remove nasal polyps, straighten a deviated septum, or use endoscopic surgery to open a good drainage channel between the sinus and your nose.
Living with your sinuses
It's nice to know that CT scans, endoscopy, and surgery are available to evaluate and treat complicated acute sinusitis and stubborn chronic sinusitis. Fortunately, garden-variety acute sinusitis will respond to much simpler treatments.
To protect your sinuses, stay well-hydrated. Avoid tobacco smoke and irritating fumes. If you have allergies, try to avoid the things that trigger symptoms. Do your best to prevent catching a cold by washing your hands properly and keeping your distance from cold sufferers. When you catch a cold, blow your nose properly to keep bacteria from flooding into your sinuses. Treat symptoms of sinusitis promptly with steam inhalation, decongestants, and nasal irrigation. If you don't recover as expected, or if you have serious sinusitis or warning symptoms, see your doctor for antibiotics and, possibly, nasal steroids.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.