Treating osteoporotic fractures of the spine
ARCHIVED CONTENT: As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date each article was posted or last reviewed. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
Several options, from pills to procedures, can help ease pain and shore up bone.
More than 1.5 million osteoporosis-related fractures occur each year in the United States, and nearly half of them are in the vertebrae, the bones of the spinal column. Vertebral fractures are twice as common as hip fractures; about 25% of postmenopausal women have had at least one. Unlike hip fractures, which almost always result from a fall, vertebral fractures usually involve little or no trauma. Vertebrae weakened by osteoporosis cannot withstand normal strain and pressure, so they may succumb to simple movement — bending over, turning quickly, or lifting a window sash.
About two-thirds of vertebral fractures have no symptoms and may go undiagnosed until they're found on an x-ray taken for some other reason. A single fracture may seem of little consequence, but having had one has long-term implications, including a higher risk of new fractures. In a study published in 2007 in The Journal of the American Medical Association, researchers for the Study of Osteoporotic Fractures found that women with a history of vertebral fracture had a fourfold greater risk of experiencing a new one during the 15-year follow-up. They also had a higher risk for other broken bones, especially hip fractures.
The cumulative effect of multiple fractures can be devastating. Chronic pain, disability, and difficulty engaging in normal activities of daily life can lead to isolation, problems with relationships, and emotional difficulties — including depression, which develops in 40% of people with vertebral fractures. Vertebral fractures also raise the risk of premature death, though not to the degree that hip fractures do.
As the population ages, the rate of osteoporotic fractures in general is expected to rise. Fortunately, we have more ways to manage these fractures than we had even 10 years ago, including procedures that relieve pain, shore up damaged vertebrae, and reduce disability.
Consequences of vertebral fractures
A vertebra isn't broken in the usual sense of the word. It doesn't snap like a twig, or like a broken leg or arm. Instead, it collapses, the way a paper cup is crushed when you step on it. The common term for this kind of break is compression fracture.
The resulting pain may be sharp or dull, and it may be felt at the site of the fracture or farther away in the sides or the abdomen. In many cases, there's little or no pain, and the chief sign is gradual loss of height or stooped posture. The amount of height loss and deformity depends on the number, location, and severity of the fractures.
Most people with vertebral fractures have one or two, commonly in the thoracic (mid-back) and sometimes in the lumbar (low back) region. One or two fractures are likely to produce a slight loss of height, but multiple fractures can contribute to a rounding of the back known as dorsal kyphosis, or dowager's hump. Caused by a number of factors, including degenerative changes in joints, disks, and bones, kyphosis can profoundly affect appearance, mobility, and health. The spine becomes progressively more misaligned. The upper body is pitched forward and rounded. The space between the ribs and pelvis closes; the chest wall is cramped; and the abdominal organs get scrunched, causing the abdomen to bulge forward. In very severe cases, breathing may be difficult, and digestion impaired.
Cumulative compression fractures can cause almost as much physical and functional disability as hip fractures. Pain can become chronic as back muscles work harder to accommodate changes in the spine. A cane or walker may be needed, and riding in a car for more than a few minutes may become unbearable.
|
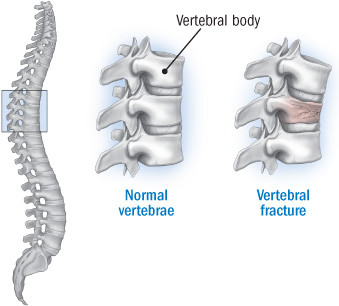
Anatomy of a vertebral fracture
When a vertebral fracture occurs, the vertebral body (the front portion of the vertebra) collapses on itself. One or two fractures can cause a loss of height; if several vertebrae collapse, it can result in a marked curvature of the spinal column. |
What to do about vertebral fractures
An x-ray of the spine can confirm the diagnosis. Vertebral compression fractures in postmenopausal women are usually caused by osteoporosis, but occasionally they result from trauma, infection, or a cancerous tumor.
Treatment for painful fractures starts with over-the-counter analgesics such as acetaminophen (Tylenol), aspirin, or ibuprofen (Advil or Motrin). Severe pain may require short-term bed rest and stronger drugs, starting with low doses of opiates, such as oxycodone (OxyContin), often combined with acetaminophen. Prolonged bed rest should be avoided, as it can contribute to bone loss and other health problems. Ice or heat packs applied to the affected area of the spine may also help.
A back brace is usually recommended to help manage pain and stabilize the spine as it heals. The brace is designed to hold the spine straighter than usual, relieving pressure on the damaged vertebrae and reducing the chance of further collapse. Healing can take up to three months. The brace shouldn't be used longer than that because it can weaken trunk muscles. Patients are usually encouraged to get gentle exercise, such as swimming or walking, as soon as they can tolerate movement. Eventually, they should add trunk muscle strengthening to their routine.
Patients should be evaluated for osteoporosis with bone mineral density testing, and osteoporosis should be treated with standard osteoporosis drugs, such as the bisphosphonates alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva). Bisphosphonates can help with acute pain, but their main benefit is improved bone mineral density. Long-term, they can reduce the rate of new vertebral fractures by as much as 50%. Injectable bisphosphonates — zoledronic acid (Reclast, Zometa) and injectable Boniva — are an alternative for women who can't take the oral form. Another bone drug, calcitonin (Miacalcin, Fortical), is less effective in improving bone mineral density but can provide some pain relief, although it's not a substitute for analgesics. The bone-building drug teriparatide (Forteo), given by injection, increases bone mineral density and lowers vertebral fracture risk.
Procedures for treating vertebral fractures
Two minimally invasive procedures — vertebroplasty and kyphoplasty — involve the injection of a medical cement to stabilize compressed vertebrae. Introduced in the United States in the 1990s, they've become increasingly available for the treatment of fracture pain that doesn't respond to more conservative therapy. According to Dr. John Pan, a radiologist at Boston's Brigham and Women's Hospital, bracing and analgesics are usually tried first "to see if the fracture heals on its own. If it doesn't and the person continues to have pain — usually after four to six weeks — that's when the procedure is considered."
There are very few controlled studies comparing the long-term effectiveness and safety of vertebroplasty and kyphoplasty — with each other or with conservative treatment. It's not clear whether either procedure improves spine stability or prevents fractures in the long run. But the main reason for these procedures is pain, and as many as 85% to 90% of people who undergo them experience immediate relief. A review of 21 studies involving 1,309 patients, published in 2007 in the journal Pain Physician, found that both techniques reduced pain by more than 50%.
No one knows exactly how these procedures do that. One theory is that the pain is largely an inflammatory response to the uneven distribution of mechanical forces caused by bone fragmentation. The cement is thought to help by restabilizing the vertebra, which reduces inflammation and thus pain. It's also possible that the cement destroys pain-conducting nerve endings in the vertebra.
Before either procedure, MRI is usually performed to determine if the patient is likely to benefit. A good candidate is one whose MRI shows the presence of bone edema, or fluid, which is associated with recent fracture. If bone edema is absent, that implies the fracture has healed and is not what's causing the pain. An MRI can also help ascertain whether a disk, the spinal cord, or other soft tissue is involved.
Both kyphoplasty and vertebroplasty are performed percutaneously (that is, through the skin), often as day surgery and under conscious sedation. If the fractures are numerous or severe, or the patient is older and in poor health — or cannot tolerate lying on his or her stomach — general anesthesia may be used. Sometimes an overnight hospital stay is necessary. Here's what's involved:
Vertebroplasty. Guided by computed tomography (CT) or fluoroscopy (real-time x-rays), a specially trained radiologist, neurologist, or orthopedic surgeon inserts a hollow needle through a small incision in the skin into the compressed portion of the vertebra. When the needle is in place, she or he injects a surgical cement (methyl methacrylate), which has the consistency of toothpaste. It's mixed with an agent that allows the physician to see its flow into the vertebra. The cement hardens within about 15 minutes. The patient is monitored for two to three hours in the recovery room before going home.
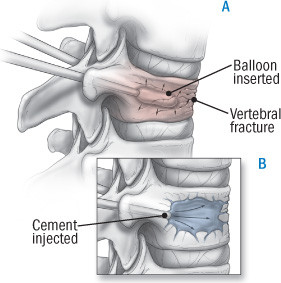
Kyphoplasty. In this procedure, which is also image-guided and performed through tiny incisions in the back, inflatable balloons are inserted through tubes in both sides of the fractured vertebra (see illustration). The balloons are inflated, creating a cavity and restoring vertebral height. They are then deflated and withdrawn and the cavity is filled with cement. The procedure takes 30 to 60 minutes for each fracture and sometimes involves an overnight hospital stay.
|
What is kyphoplasty?
Kyphoplasty is a two-step process. First, a tubelike device with a balloon at the end is inserted into each side of the collapsed vertebra (A). The balloons are then inflated, creating a cavity and restoring vertebral height. The balloon is withdrawn and cement is injected, filling the cavity (B). |
What are the risks?
In well-trained and experienced hands, vertebroplasty and kyphoplasty are generally quite safe. But anesthesia always creates risks, nerves can be damaged during needle placement, and any procedure that involves cutting into the skin raises the possibility of bleeding and infection.
Cement leaks can be a concern, but with real-time monitoring using CT or fluoroscopy, the physician can spot them early and stop the injection. The main worry is that cement might leak into places where it could cause serious problems. In the spinal canal, for example, it can press on the spinal cord, or if it gets into the bloodstream, it can cause clots that travel to the heart and lungs. But these complications are extremely rare in the treatment of osteoporosis-related vertebral fractures. (Compression fractures resulting from tumors, infection, or trauma can be trickier and have a somewhat higher complication rate.)
Selecting the right patients helps avoid complications. For example, someone with a compression fracture greater than 70% of the height of the vertebral body isn't a good candidate for either procedure, says Dr. Pan, because there's too little room for the needle and cement, and leaking becomes more likely. Another red flag is a compression fracture on the spinal-canal side of the vertebra, where a cement leak could impinge on the spinal cord.
The long-term effects of cement in a vertebra are unknown; researchers are investigating the possibility that it increases the risk of fractures in adjacent vertebrae, possibly through a change in mechanical forces.
Some physicians think patients should undergo vertebroplasty or kyphoplasty as a first choice, instead of waiting four to six weeks to judge the effect of pain medications, bracing, and bed rest. But most believe that until we know more about the risks, benefits, and long-term effects of these procedures, trying conservative measures first seems prudent. Finally, if you are considering one of these techniques, be sure that the hospital has extensive experience with it — and top-flight imaging equipment.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.