When nerves get damaged
Peripheral neuropathy causes strange feelings of numbness and sometimes pain.
- Reviewed by Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing

We've all had a foot fall asleep because of the way we have been sitting or standing. The abnormal pressure pushes on nerves and compresses the blood vessels that supply them. The nerves react to their distress by sending signals that cause an unpleasant, even painful, tingling sensation. But it's a temporary situation: the pins-and-needles go away after we change position, so blood vessels open up and the pressure is off the nerve – unless you suffer from peripheral neuropathy.
For people with peripheral neuropathy, that tingling sensation — along with pain, burning, numbness, and other uncomfortable feelings — doesn't go away so easily. Peripheral neuropathy symptoms aren't a response to a fleeting lack of blood supply and pressure, but to injury or irritation of the nerves. Depending on which nerves are affected and the extent of the problem, muscles may weaken and eventually atrophy. And if the nerves of the autonomic nervous system are involved, basic functions like bladder and bowel control may be impaired, and the consequences even more serious.
What causes peripheral neuropathy?
The causes of peripheral neuropathy are many and various. In the United States, diabetes leads a list that includes excessive alcohol consumption, nutritional deficiencies, a medication side effect, exposure to toxic chemicals, and autoimmune disorders that launch errant attacks on the nervous system. Some infectious diseases can result in neuropathy, such as Lyme disease, and in some parts of the world, leprosy is an important cause. There are inherited conditions that produce debilitating neuropathy.
Fairly often, though, the origin can't be identified, which can be frustrating (to put it mildly) for doctors and patients alike. Those cases are called idiopathic peripheral neuropathy — idiopathic being the medical term for a disease from an unknown cause.
One of the reasons idiopathic cases can be so troubling is that whenever possible, treatment of peripheral neuropathy zeroes in on the underlying cause in hopes that eliminating or at least ameliorating the cause will have the same effect on the neuropathy it's producing. So, for example, if the neuropathy is from diabetes, tighter control of blood sugar may reduce the severity of symptoms and perhaps keep it from getting worse.
The other strategy is to tackle the problem at the level of symptoms with a variety of medications that seem to quiet down the nervous system and perhaps alter how signals from damaged nerves are received in the brain. However, most of the medications used in this way are prescribed "off-label," which means that they were approved by the FDA for other purposes. Tricyclic antidepressants, an older class of antidepressant medications, are often quite effective, as are several medications that were originally approved to control the seizures from epilepsy.
Stocking and glove
Peripheral neuropathy symptoms often start in the feet and spread up the legs. The hands and arms are affected next. |
Sorting out the peripheral neuropathy terminology
The terminology surrounding peripheral neuropathy can be confusing, especially if you are new to it. Peripheral refers to the peripheral nervous system, which consists of the vast network of nerves that connect our sense organs, muscles, glands, and internal organs to the central nervous system, which consists of the brain and spinal cord. Peripheral neuropathy therefore is used to describe any situation involving damaged or disrupted nerves outside the brain and spinal cord. Polyneuropathy refers to conditions that affect many peripheral nerves at once. And, not surprisingly, mononeuropathy describes conditions that affect a single nerve — carpal tunnel syndrome, for example.
Mononeuropathy multiplex is a user-unfriendly term that you may only run across in medical textbooks or in online searches of the medical literature. It refers to situations when a few distinct nerves in separate areas of the body are damaged at different times. It's sometimes used to draw a distinction with polyneuropathy, which tends to involve groups of nerves.
Part of the reason medical terminology can be such a briar patch is that terms aren't used consistently or have overlapping meanings. For example, neuritis means inflammation of the nerves. Many medical reference books say it is synonymous with neuropathy, although neuropathy is increasingly the favored term and has a broader meaning. Neuralgia is pain generated by a nerve, so it can be an aspect of neuropathy, but many neuropathies produce sensations other than pain.
Damaged wires and insulation
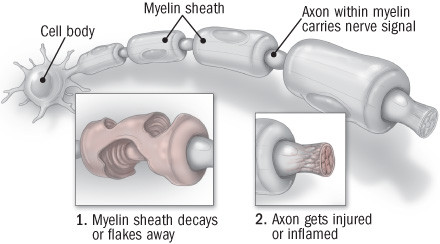
The analogy isn't perfect and is hardly original, but one way to gain a quick understanding of neuropathy is to think of the peripheral nervous system as a complicated wiring system for carrying messages to and from the brain and spinal cord. The "live wires" in the system are the axons that connect one nerve cell to another (see the illustration). And, like wiring, those axons are wrapped in an insulating material — not rubber or plastic, of course, but a fatty substance called myelin. As the peripheral nervous system branches out and the nerves get smaller and smaller, axons of smaller branches often lack myelin.
Most peripheral neuropathies are the result of damage to either the message-carrying axons or to the insulating sheath of myelin, although sometimes both occur.
Two types of nerve damage
|
The stocking-and-glove pattern
Peripheral neuropathy from diabetes or excessive alcohol is mainly the axonal variety. The far ends of the longest axons in the body are usually affected first. As a result, symptoms often start in the extremities — the feet and toes, followed by the hands and fingers. At first, there's vague discomfort and a loss of feeling that is sometimes compared to having a sock bunched up in a shoe or the feet having a wooden feeling. As the neuropathy worsens, which can occur quite gradually over many years, these and other sensations tend to travel up the leg and arms in a pattern referred to as "stocking and glove."
In addition to numbness, the symptoms of axon-related neuropathy include burning sensations, pins-and-needles, and outright pain with a stabbing quality. Some people experience allodynia — pain from what would ordinarily be perfectly harmless stimuli like a light touch on the skin. Eventually, the axons of nerves in other parts of the body may be affected, so symptoms are felt around the ribs and chest and sometimes the top of the head.
Toxins and some drugs also tend to cause axonal damage, and — particularly if it happens suddenly and in large doses — the predominant symptom may be pain, not numbness.
Guillain-Barre syndrome, an autoimmune disorder, is an example of a condition that first damages myelin, not axons. Muscle weakness, accompanied by a tingling sensation, is the main symptom. Guillain-Barre often (but not always) comes on after a lung or gastrointestinal infection.
Direct physical injury is often the cause of the mono-neuropathic conditions that involve a single nerve. Typically, the injury to the nerve comes from prolonged pressure on, or irritation of, a nerve near the skin or a bone. Carpal tunnel syndrome, for example, is the result of the pressure on the median nerve in the wrist that supplies the thumb side of the hand. Saturday night palsy (palsy means paralysis) is the colorful nickname for damage to the radial nerve in the arm. The nickname comes from situations when the nerve gets compressed because people have fallen asleep with an arm slung over the back of a chair or tucked under their heads after a night of revelry.
Tests of nerves
The diagnosis of peripheral neuropathy begins with questions to the patient about the symptoms, when they started, how they have changed, and so on. Doctors should also ask about a family history of neuropathy and conditions that are known to cause neuropathy, such as diabetes.
There are also tests to assess nerves and nerve function. Nerve conduction tests involve stimulating nerves with a very mild electrical shock, which sends an electrical signal down the nerve. The test measures the speed with which the signal travels. Slower speeds can suggest nerve damage. Electromyography is a test that measures the electrical activity of muscle membranes while the muscle is at rest and during voluntary activity.
Occasionally, doctors will order a biopsy. Small pieces of skin can be inspected for the density of small nerve fibers, and the nerves themselves can be biopsied. The information gleaned from these and other tests can help doctors determine if the neuropathy is caused by inflammation or damage to axons or to myelin, which can shed some light on the underlying cause.
Whether these nerve tests need to be done depends on the other information at hand. If, for example, someone with diabetes develops mild neuropathic symptoms in the classic stocking-and-glove pattern, diagnostic nerve tests might not be necessary. A more direct and less expensive approach to diagnosing the problem would be a simple blood test to show if blood sugar or other factors had gotten out of control.
Treating the treatable cause of peripheral neuropathy
In many medical conditions, it's more difficult to identify and treat the cause than the symptoms. With peripheral neuropathy, it can be the other way around: once the cause is removed or at least reined in, the nerves may heal. and the symptoms ease up. Peripheral neuropathy from diabetes is a prime example. Blood sugar levels can be controlled with diet, exercise, and, if need be, medication. Better blood sugar control can help stop neuropathy from getting worse. Another example of a treatable cause of neuropathy is excessive alcohol use: heavy drinkers can cut back.
This perhaps paints too rosy of a picture. In many cases, even when the cause is known, people with peripheral neuropathy need relief from the symptoms, especially if one of them is pain. Unfortunately, conventional painkillers like ibuprofen or aspirin may not be very effective.
Instead doctors often prescribe medications originally designed to treat seizures and depression. Examples of alternatives include pregabalin (Lyrica), gabapentin (Neurontin), amitriptyline (Elavil), desipramine (Norpramin), and nortriptyline (Pamelor). The side effects (drowsiness, dry mouth, weight gain) can be a drawback but they may be a reasonable trade-off if there's relief for troubling symptoms, especially pain.
Many people with peripheral neuropathy say yoga, acupuncture, and other somewhat unconventional treatments have done wonders. Supporting data are scarce, but these alternative approaches might be worth a try as long as there's little risk of harm.
Illustrations by Scott Leighton
About the Reviewer

Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.