Lung cancer: Not just for smokers
People who never smoked may have a different form of the disease that responds better to a new generation of targeted medications.
"Did he smoke?"
That's often the first response to news that someone has lung cancer. It's an understandable reaction: We've been reading and hearing about the link between smoking and lung cancer ever since the 1964 Surgeon General's report. Cancer epidemiologists estimate that 85%–90% of those who die from lung cancer in the United States were smokers.
But what of the remaining 10%–15%? Some experts estimate that as many as 15,000 Americans die each year from lung cancer even though they have never smoked. The most famous recent case was Christopher Reeve's widow, Dana Reeve, who died in 2005. If never-smokers' lung cancer were a separate category, it would be among the top 10 most lethal cancers in the country, ranking somewhere near ovarian cancer.
Secondhand smoke is undoubtedly a factor in many cases. According to one estimate, every year about 3,000 Americans get lung cancer from breathing in secondhand smoke, although evidence suggests that exposure is declining as workplace and restaurant smoking bans become more common.
Even when you factor in secondhand smoke, there's a sizable group of lung cancer patients whose disease can't be easily traced to tobacco.
Its own disease
Until recently, doctors had little reason to view lung cancer affecting never-smokers as a separate entity. Diagnosis and treatment are the same, regardless if patients smoked or not. Never-smokers may have responded slightly better to treatment than smokers, but doctors had no way of determining whether there were inherent differences in the cancers of smokers and never-smokers, or if those who never had smoked were just healthier, perhaps because they didn't have the cardiovascular illnesses that smoking causes.
Now, however, there's growing recognition that in certain key respects, never-smokers' lung cancer may be a distinct disease. Two cancer medicines — gefitinib (Iressa) and erlotinib (Tarceva) — are more effective in people who never smoked, and researchers have identified genetic differences that may explain why. As part of a clinical trial, doctors at the Harvard-affiliated Dana-Farber Cancer Institute in Boston are testing the lung cancer tumors of never-smokers and former smokers with relatively light habits. If the researchers find certain genetic mutations, those patients receive Tarceva as their first-line therapy (ordinarily, it's only used after conventional chemotherapy has failed). Similar studies are under way at Massachusetts General Hospital using Iressa.
Dr. Pasi A. Jänne, a researcher at Dana-Farber, says these trials are the "first example of personalized medicine in lung cancer." Personalized medicine is the catchphrase for efforts to tailor medical treatment to a patient's individual genetic profile.
|
Response rates to gefitinib (Iressa) |
|
|
Groups |
Response rate (shrinkage of tumor) |
|
Women vs. men |
19% vs. 3% |
|
Japanese vs. white |
27.5% vs. 10.4% |
|
Adenocarcinoma vs. other types of lung cancer |
13% vs. 4% |
|
Never-smokers vs. current and former smokers |
36% vs. 8% |
|
Source: Adapted from Journal of Clinical Oncology, May 10, 2005, p. 3229 |
|
Who is affected?
Epidemiologists have had some difficulty getting a handle on nonsmokers' lung cancer. Smoking history isn't necessarily part of official death records. Researchers have used reports by relatives and hospital records to sort out smokers from nonsmokers, but that kind of evidence can be incomplete.
In 2005, though, a number of studies of never-smokers were published. Epidemiologists at the American Cancer Society (ACS) reported results from one of the largest studies so far. They had access to data from two huge ACS cancer-prevention studies that included about 940,000 people who said they had never smoked. Smoking status was ascertained from questionnaires people filled out when they signed up to be in the prevention studies. Mortality rates were calculated from deaths reported during about 12 years of follow-up.
The ACS researchers' conclusions challenged some commonly held beliefs about never-smokers' lung cancer. They found that the lung cancer mortality rate is actually higher for male never-smokers, although there are more female patients because there are so many more women age 60 or over in the never-smoker category. They also found that the mortality rate is higher for African American women than for white women. And while some studies have found that the number of cases of never-smokers' lung cancer is going up, the ACS researchers' analysis found no evidence of such an increase.
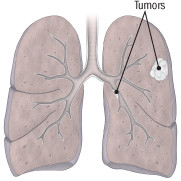
Inherited risk
In another study, published in the Journal of Clinical Oncology, researchers in Singapore reported that almost a third (32.4%) of the lung cancer patients in that country had never smoked, which is similar to the proportion in Japan. They found that patients who never smoked were diagnosed with more advanced cancers than smokers, perhaps because doctors aren't looking for the disease. Most (68.5%) of the never-smokers were women and had adenocarcinomas (see illustration). How many of these cancers might have been caused by secondhand smoke is impossible to say. The researchers said they couldn't document passive smoking.
|
Lung cancer today
Adenocarcinoma is now the most common type of lung cancer. Tumors grow in the smaller airways toward the outer edges of the lung and under membranes lining the bronchi. Once seen mainly in never-smokers, it's increasingly seen in smokers. |
Lung cancer runs in families, but so does smoking, so it doesn't jump out as an inherited, genetic condition. But Japanese researchers reported in the October 2006 issue of the journal Chest that family history was a stronger risk factor among never-smokers than among smokers, suggesting perhaps that never-smokers' lung cancer may indeed have a significant inherited component.
Drugs get smarter
FDA approval of imatinib (Gleevec) in May 2001 was heralded as the beginning of a new era in cancer treatment that would feature "smart" drugs designed to zero in on aberrant proteins found only in cancer cells. Their selectivity would not only make them more effective, but also produce fewer side effects because noncancerous cells would be largely unaffected. What sometimes got lost in the excitement was that Gleevec worked against relatively rare cancers (chronic myelogenous leukemia and gastrointestinal stromal tumors). In contrast, gefitinib (Iressa) targeted epidermal growth factor receptors (EGFRs), which are found in many cancers. They raised hopes for Gleevec-like drugs for more common forms of cancer.
But there was a major snag: Iressa shrank tumors in only about 10% of the lung cancer patients who took the drug. "If you look on the surface of lung cancer cells, 90% of them have this EGFR receptor," says Dr. Jänne. "But only 10%–15% of patients responded. That was the clinical paradox: If the receptor is there, why doesn't everyone benefit?"
When researchers examined study results in more detail, they found that the lung cancers of certain types of people were more likely to respond to Iressa and Tarceva. Women's tumors had a noticeably better response rate than men's, for example. Japanese patients fared better than average. And, interestingly, so did people who hadn't smoked. In one trial, the median survival time of never-smokers more than doubled (from 10 months to 22.5 months) when Tarceva was added to conventional chemotherapy.
The favorable results in Japanese and other East Asian patients have led to a flurry of Iressa and Tarceva studies in Asia. Researchers also began searching for variations in the genes of lung cancer cells that might explain the divergent responses. Dr. Jänne says it now appears that 85% of tumors that respond to Iressa and Tarceva have cells with one of two mutations. In the clinical trial at Dana-Farber, researchers are testing lung cancer patients whose tumors have the greatest chance of having those two mutations — a group that includes nonsmokers — and treating them with Tarceva if those mutations are found.
Overcoming resistance
Some of the bloom came off Gleevec's rose when doctors found that patients developed resistance to the drug. Fortunately, a second generation of drugs has been developed that can be used after resistance occurs. In 2005, the FDA approved two of them, sunitinib (Sutent) and dasatinib (Sprycel). These drugs are not quite as "single-minded" as Gleevec and target multiple proteins, not just one.
Resistance is also a major limitation for both Iressa and Tarceva. Virtually all patients who respond to the drugs develop resistance within 14 months or so. In about half of these patients, researchers have identified a genetic mutation that appears to be responsible. In 2005, Dr. Jänne and his colleagues reported research results showing that even a small number of the mutated genes could cause resistance, which may make accurate testing difficult. But the hope is that drug developers will find an agent that can deactivate such resistance-causing genes and that testing for them will become a routine part of personalized medicine.
Redrawing the boundaries
For the foreseeable future, smoking will continue to be the main cause of lung cancer, so smoking cessation programs and getting young people not to smoke remain priorities. At the same time, the large group of lung cancer patients who never smoked should remind us that we need to look beyond the usual risk factors and disease categories. With the advent of genetic testing, as well as some old-fashioned epidemiology, traditional diagnostic and treatment boundaries are in flux and new entities — like never-smokers' lung cancer — are getting added to the map. Let's hope the science of prevention and treatment can keep up.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.