Counting steps is good — is combining steps and heart rate better?

Appendix pain: Could it be appendicitis?

Can saw palmetto treat an enlarged prostate?

How does Ozempic work? Understanding GLP-1s for diabetes, weight loss, and beyond

Zinc: What it does for the body, and the best food sources

Respiratory health harms often follow flooding: Taking these steps can help

Tips to leverage neuroplasticity to maintain cognitive fitness as you age

Can white noise really help you sleep better?

Celiac disease: Exploring four myths

What is prostatitis and how is it treated?
Heart Health Archive
Articles
What is long QT syndrome?
Ask the doctor
Image: © Shidlovski/Getty Images
Q. I was recently diagnosed with long QT syndrome, which was apparently caused by a medication I was taking. But I understand that there are also genetic causes for this problem. Can you tell me more about this disorder?
A. Long QT syndrome is a rare disorder of the heart's electrical system. Electrical signals coordinate your heartbeat, telling the heart to contract and relax to pump blood. After each beat, the heart's muscle cells are busy recharging themselves for the next contraction by moving sodium, potassium, and calcium through tiny pores on their surfaces.
Treatments for breast cancer may harm the heart
But surveillance and other strategies — especially exercise — can limit the risk.
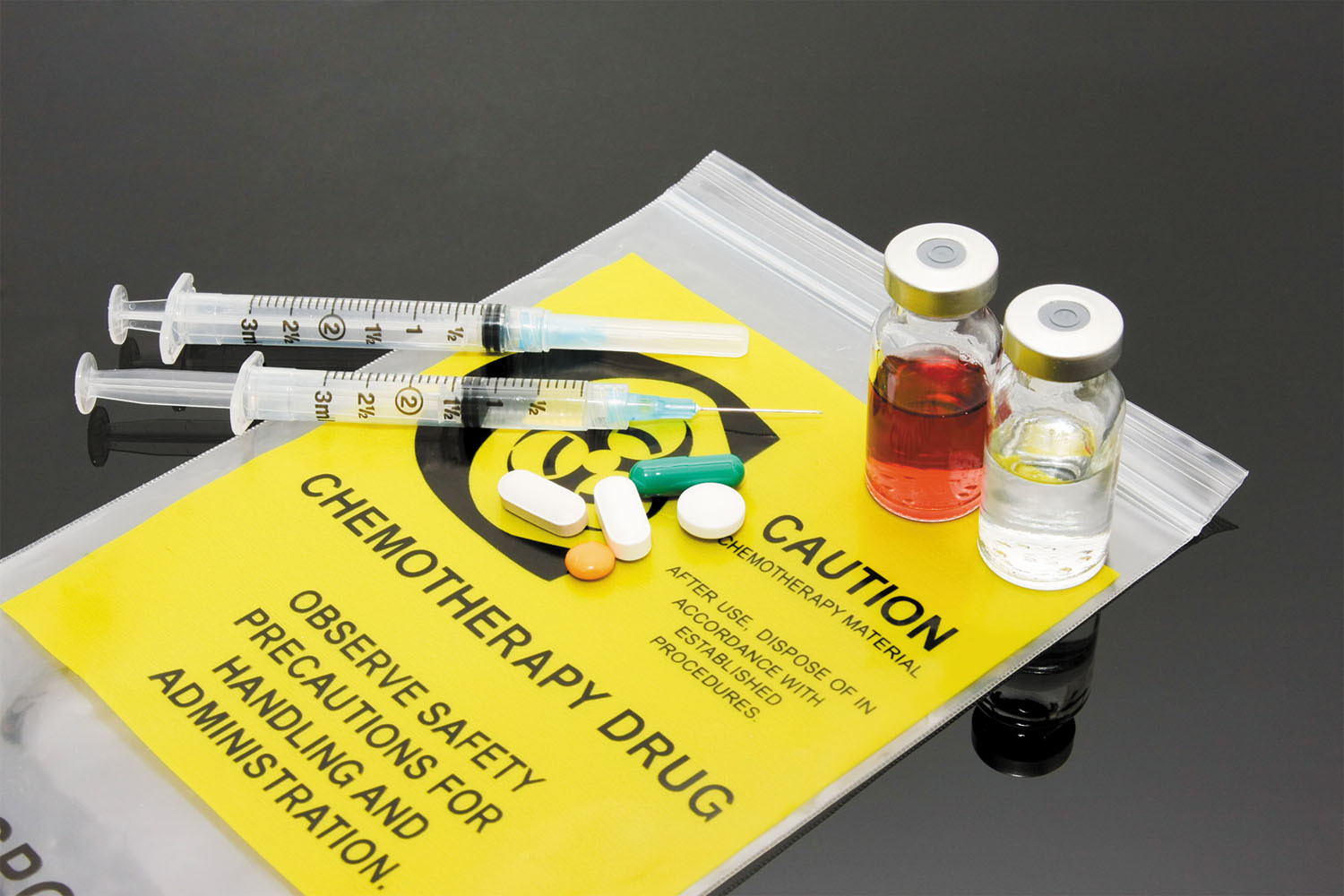
Image: © Khuong Hoang/Getty Images
Better treatments for breast cancer have contributed to the growing number of breast cancer survivors, now about three million in the United States. However, these women may face a heightened risk of heart disease from the cardiotoxic effects of chemotherapy and radiation, according to a statement from the American Heart Association in the Feb. 20, 2018, issue of Circulation.
Doctors have long known that certain cancer drugs can decrease the heart's pumping ability, especially doxorubicin (Adriamycin) and trastuzumab (Herceptin), two common treatments for breast cancer. Many women receive radiation therapy as well, which can cause heart tissue to scar or stiffen, possibly leading to valve disorders, coronary artery disease, or other heart problems. But specialists who focus on keeping the heart healthy during and after cancer treatment — known as cardio-oncologists — can offer strategies to both prevent and treat heart damage from cancer therapy.
Vegetable of the month: Red cabbage
Image: © pjohnson1/Getty Images
Slivers of this vibrantly colored vegetable, also known as purple cabbage, are sometimes added to cabbage salads and coleslaw. But why not add red cabbage to any salad — or even make it the star ingredient?
Red cabbage contains substances called anthocyanins, which are responsible for the red-orange to blue-violet colors found in many fruits and vegetables. Population-based studies have linked a higher intake of anthocyanins and other so-called phytochemicals to a lower risk of cardiovascular disease.
Traffic noise linked to higher heart disease risk
Research we're watching
Image: © u_/Getty Images
Roaring jets, rumbling trains, and revving automobiles may have a detrimental effect on your cardiovascular health.
According to a review article in the Feb. 13, 2018, Journal of the American College of Cardiology, many studies have observed a connection between transportation-related noise and a slightly higher risk of high blood pressure, coronary artery disease, stroke, and heart failure. The association persists even after adjustment for possible confounding factors, such as air pollution and socioeconomic status.
Standing vs. sitting: Fewer pounds, less heart disease?
Research we're watching
Compared to sitting, standing burns slightly more calories — about 0.15 calories per minute. But that tiny difference adds up: a person who weighs 143 pounds could burn an extra 54 calories per day by standing instead of sitting for six hours, as researchers report in the Jan. 1, 2018, European Journal of Preventive Cardiology.
Assuming that person kept eating the same number of calories per day, that translates to 5.5 pounds of weight loss after one year. The estimate comes from data pooled from 46 different studies.
Weight loss and exercise may ease atrial fibrillation
Research we're watching
For people with atrial fibrillation, losing a little weight and getting exercise may improve their symptoms, according to a review published online Feb. 7, 2018, by The American Journal of Cardiology.
Atrial fibrillation (or afib) is a common heart rhythm disorder marked by a quivering or fluttering heartbeat, which can cause dizziness and breathlessness. Other symptoms include fatigue, weakness, and fainting.
Can you get heart problems despite a healthy lifestyle?
Ask the doctor
Q. Is it possible to have heart problems, even if you live a healthy lifestyle? Or to avoid heart problems, even if you don't live a healthy lifestyle?
A. Life contains no guarantees: yes, even if you live a healthy lifestyle you still can develop heart problems — particularly if you have been born with "bad" genes that make you vulnerable to heart disease.
The wholesome goodness of grains
Eating more whole grains is linked to a lower risk of heart disease.
Image: © Bigacis/Getty Images
The word "refined" often describes things that have been stripped of impurities or other unwanted elements. But when it comes to wheat, rice, and other grains, the refining process instead removes the most healthful parts of these nutritious foods.
For example, white flour and white rice have far less of the vitamins, minerals, healthy fats, fiber, and other plant-based chemicals called polyphenols found in whole-wheat flour and brown rice. The combination of those beneficial nutrients may explain why people who eat more whole grains have a lower risk of developing and dying from heart disease.

Counting steps is good — is combining steps and heart rate better?

Appendix pain: Could it be appendicitis?

Can saw palmetto treat an enlarged prostate?

How does Ozempic work? Understanding GLP-1s for diabetes, weight loss, and beyond

Zinc: What it does for the body, and the best food sources

Respiratory health harms often follow flooding: Taking these steps can help

Tips to leverage neuroplasticity to maintain cognitive fitness as you age

Can white noise really help you sleep better?

Celiac disease: Exploring four myths

What is prostatitis and how is it treated?
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up