New thinking about plaque in arteries that feed the brain

Want to prevent shifting teeth? Maybe you need retainers

What you need to know about the new dietary guidelines

Food that’s healthier for people and planet can be cheaper, too

New evidence that polyphenol-rich foods help the heart

8 simple ways to reduce ultra-processed foods in your diet

How to curb your stress eating

How to spot Parkinson’s disease symptoms

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux
Medications Archive
Articles
Pay less for heart drugs without using insurance?
Research we're watching
Image: © Gligatron/Getty Images
Do you take generic drugs to lower your blood pressure or cholesterol? You may save money by paying out of pocket at Walmart instead of a paying a Medicare prescription copay, according to an analysis in the July 24 Annals of Internal Medicine.
Walmart (and a number of other large chain stores) offer generic drug discount plans; they sell 30-day supplies of popular generic drugs for $4.
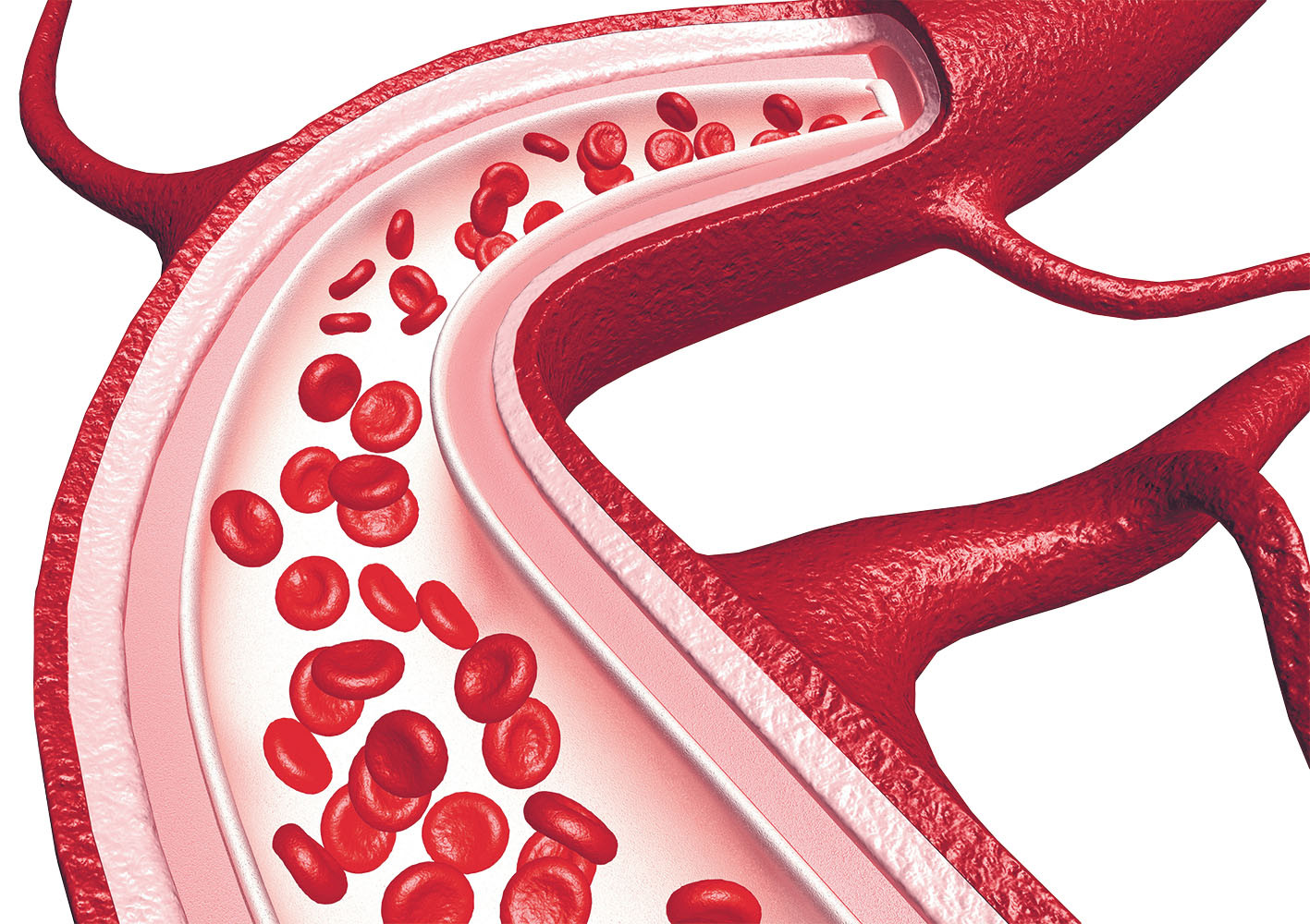
More antidotes for newer blood thinners
New medications add advantages to treatments that help prevent stroke, pulmonary embolism, and deep-vein thrombosis.
Image: © Mohammed Haneefa Nizamudeen/Getty Images
The wait is over for an antidote to stop rare uncontrolled bleeding linked to some newer blood thinners. The FDA approved andexanet alfa (AndexXa) on May 3, 2018. It's the first and only antidote to reverse bleeding in people taking apixaban (Eliquis), rivaroxaban (Xarelto), or edoxaban (Savaysa).
Another newer blood thinner — dabigatran (Pradaxa) — already has an approved antidote called idarucizumab (Praxbind). A dose of vitamin K is used to reverse the action of warfarin (Coumadin), a blood thinner used routinely for more than half a century and, until recently, the only such option for most people.
Depression risks in the medicine cabinet
News briefs
Are you taking a medication that has depression or suicidal thinking as a potential side effect? One or both risks have been linked to use of more than 200 prescription and over-the-counter pills, including medicines that treat high blood pressure, heartburn, pain, and headaches. The more of these drugs you use, the higher the likelihood that you'll experience depression, suggests a study published June 12, 2018, in The Journal of the American Medical Association. Working with five surveys conducted over a nine-year period, researchers evaluated health information from 26,192 adults. About 37% of them reported taking such medications. Of individuals taking three or more of the medications with depression as a possible side effect, about 15% reported depression, compared with about 5% in people not using those medications. Even for people already taking an antidepressant, the addition of one or more of the identified medicines was linked to higher rates of depression. This study was based on surveys, so it didn't prove that the medications caused the reported depression. Nonetheless, if you think you're depressed (and have symptoms such as apathy, hopelessness, changes in sleep or eating habits, and persistent fatigue), ask your doctor if any of the medicines you are taking may be responsible.
Image: © Tero Vesalainen | GettyImages
Your health through the decades
These strategies keep you healthy and safe through your 60s, 70, and 80s.
Image: © kali9/Getty Images
After age 60, men tend to get thrown together — the so-called 60-and-older group — even though most are quite different in terms of their health.
"While many men are still very fit well into their 60s, 70s, and 80s, others face health challenges and chronic diseases that make daily living difficult," says Dr. Howard LeWine, assistant professor of medicine at Harvard Medical School.
Arthritis drugs do little for sufferers’ mental health
In the journals
Many people with rheumatoid arthritis (RA) also deal with ongoing depression and anxiety related to their pain and disability. While drugs used to treat the disease help alleviate the joint pain and stiffness, a recent study suggests they may not extend to improving patients' mental health.
The findings, published online June 6, 2018, by Arthritis & Rheumatology, reviewed more than 70 clinical trials and found only a small association between various drugs used for RA, such as adalimumab (Humira), rituximab (Rituxan), abatacept (Orencia), and tocilizumab (Actemra), and mental health outcomes in patients.
Early therapy helps people with low back pain avoid medication
In the journals
If you suffer from low back pain and want to avoid taking strong pain medication, you might want to consult a physical therapist first, suggests a recent study published online May 23, 2018, by Health Services Research.
Researchers reviewed insurance claims for approximately 150,000 adults, ages 18 to 64, who had been newly diagnosed with low back pain. They found that those who first consulted a physical therapist had an 89% lower probability of receiving an opioid prescription compared with those who saw another type of medical provider. They were also less likely to have an MRI or CT scan or to seek out emergency care for their pain.
FDA approves first migraine prevention drug
News briefs
Encouraging news for people who suffer with migraines: in May, the FDA approved erenumab (Aimovig), the first medication aimed at preventing these debilitating headaches. Current medications to treat migraines were actually designed to control other conditions, such as seizures or an irregular heartbeat; their side effects (like sexual dysfunction and fuzzy thinking) often cause people to skip treatment. Erenumab offers a new approach. Injected once a month, it works by blocking a molecule (calcitonin gene-related peptide) involved in migraine attacks, and compared with other drugs, it appears to have fewer side effects (primarily constipation and injection site reactions). "This drug is for people who have more than four migraines per month, but it won't take migraines away entirely," says Dr. Gad Marshall, a neurologist at Harvard-affiliated Brigham and Women's Hospital. Clinical trials suggest it can reduce frequency by one or two migraines per month, or even more in some people. "For people with frequent debilitating migraines it could be a game changer," says Dr. Lee Schwamm, a neurologist at Harvard-affiliated Massachusetts General Hospital. "But erenumab is expensive, and it will take time to find out if it's effective and safe over the long term."
Getting the most out of your heart medications
These drugs help prevent potentially life-threatening events. Make sure you're taking them correctly.
Image: © SelectStock/Getty Images
Recently, a Heart Letter subscriber emailed us this query: "Does taking your blood pressure medication at night protect the heart more than if you take it in the morning? If so, why?"
Maybe you've wondered the same thing, or have other questions about the drugs you take to prevent or treat heart disease. In addition to blood pressure pills, these include drugs to lower cholesterol and to prevent blood clots.
An eye on glaucoma drugs
Two recent drugs have opened new treatment opportunities for this common eye disease.
Glaucoma is a leading cause of blindness in people over age 60, and it's estimated that the number of new cases will more than double over the next few decades. "There is no cure for glaucoma once it appears, so treating it at its earliest stages can help save your vision," says Dr. David Solá-Del Valle, an ophthalmologist with Harvard-affiliated Massachusetts Eye and Ear.
Once diagnosed, glaucoma is treated with eye drops to reduce pressure inside the eye by lowering the amount of fluid or improving fluid drainage. They can keep glaucoma from getting worse and hopefully avoid the need for surgery to correct this drainage problem.

New thinking about plaque in arteries that feed the brain

Want to prevent shifting teeth? Maybe you need retainers

What you need to know about the new dietary guidelines

Food that’s healthier for people and planet can be cheaper, too

New evidence that polyphenol-rich foods help the heart

8 simple ways to reduce ultra-processed foods in your diet

How to curb your stress eating

How to spot Parkinson’s disease symptoms

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up