Managing common vulvar skin conditions
Proper diagnosis and treatment are vital to get relief from vulvar itching and other irritating conditions.
- Reviewed by Toni Golen, MD, Editor in Chief, Harvard Women's Health Watch; Editorial Advisory Board Member, Harvard Health Publishing; Contributor
Many women have been primed to think no further than "itch equals yeast infection." But the vulva, which is the external genital area surrounding the vagina, is subject to a range of skin problems, many of them inadvertently self-inflicted.
And with age, the decline in estrogen after menopause means women become more prone to a variety of conditions that irritate vulvar skin. These conditions aren't getting the medical attention they need — and women aren't getting the relief they deserve.
Vulvar skin conditions and their treatment
Several vulvar skin conditions are familiar from other areas of the body but may be difficult to recognize when they appear on the vulva. These include the following:
Eczema
This inflammatory skin condition disrupts the skin's surface, causing red patches and thin cracks, weeping, and crust formation.
On the vulva, crusts are less likely, but eczema may initiate a cycle of vulvar itching and scratching that leads to lichen simplex chronicus — thickened and intensely itchy skin.
If eczema affects an area of the vulva called the vestibule (the smooth skin next to the vaginal opening and upward toward the clitoris), it may cause stinging and burning. Sometimes eczema appears in early childhood and its cause is unknown. More often, it begins with exposure to an irritant or allergen.
To diagnose vulvar eczema, the clinician will ask about your symptoms; your history of eczema, allergy, and related conditions; your vulvar cleansing habits; and any products the vulva has been exposed to. During the exam, she or he will look for redness, scaling, cracking, and thickening.
All eczema requires gentle skin care. In simple cases, patients use topical corticosteroid ointments twice a day for two to four weeks, and then gradually reduce the frequency until the symptoms are gone. Severe cases may require a short course of a potent corticosteroid ointment.
During treatment, you must stop scratching, so your clinician may prescribe an antihistamine (usually taken at night to prevent daytime drowsiness). A cold pack can also help relieve itching.
Psoriasis
Psoriasis is a common condition in which new skin cells are produced too rapidly, leading to thickened, scaly patches of inflamed and red skin on various parts of the body.
On the vulva, skin surfaces are usually too moist for dry scaling, so psoriasis is more likely to appear in the form of pink patches with defined edges. It most commonly affects the labia majora, and there may produce dry, scaly, and itchy patches of skin in the hair-bearing areas. If the skin cracks open, irritation or infection may result.
You may have treated psoriasis outbreaks elsewhere on your body with remedies that may be too harsh to be used on the vulva. Your clinician may prescribe a topical steroid cream or ointment.
Lichen sclerosus
Although it can occur elsewhere on the body, this inflammatory skin disorder usually affects the vulvar or anal area in postmenopausal women. By some estimates, one in 30 older women has lichen sclerosus. It's especially common in women with psoriasis.
Itching is usually the first symptom, and it may become severe enough to disrupt sleep and other activities. During an examination, the clinician may notice white (sometimes crinkly or shiny) patches. Some may contain tears or red areas from bleeding (often the result of scratching), and these areas may be painful and sting. As the disease progresses, there's a danger that vulvar tissues will scar and shrink.
Lichen sclerosus is diagnosed by its appearance and sometimes by biopsies. No matter how mild the symptoms, it should be treated to prevent progression. The usual treatment is application of a high-potency corticosteroid ointment for several weeks, then slowly tapering the dose.
Women also need regular examinations after treatment for lichen sclerosus because the condition can make affected skin more likely to develop skin cancer. Early treatment and prompt attention to new lesions or nonhealing sores in the area will reduce the risk further.
Lichen planus
This skin condition, believed to result from an overactive immune system, can affect the vulva, the vagina, the inside of the mouth, and other skin surfaces. In most areas of the body, lichen planus causes itchy purple bumps sometimes streaked with white.
On vulvar skin, the most common symptoms are soreness, burning, and rawness. The vulva may appear pale or pink, sometimes with a white lacy pattern. If the vulvar skin breaks down, the eroded areas appear moist and red. Lichen planus often affects the vagina as well, causing a sticky yellow discharge and erosions that can make intercourse painful.
Eventually, lichen planus can affect underlying as well as surface tissues, and produce scarring that alters the vulva's shape, sometimes leading to the virtual disappearance of the labia minora.
Lichen planus is diagnosed by its appearance (although it can be difficult to distinguish from atrophy caused by a lack of estrogen or the excessive use of steroids), and the diagnosis is confirmed with a biopsy. The condition may start as a reaction to certain medications, so be sure to tell your clinician about any drugs you take.
The most common initial treatment is high-potency topical steroid medication. Unfortunately, lichen planus is persistent and likely to require long-term maintenance treatment.
Irritants and allergens that can affect the vulva
Many things can cause an allergic reaction or irritate vulvar skin. Here are some of the leading suspects.
Irritants
On exposure, irritants can cause immediate stinging or burning. Irritants include:
- soap, bubble baths and salts, detergent, shampoo, conditioner
- adult or baby wipes
- panty liners and their adhesives
- nylon underwear, chemically treated clothing
- vaginal secretions, sweat, and urine
- douches, yogurt
- spermicides, lubricants
- perfume, talcum powder, deodorants
- alcohol and astringents
- scented toilet paper
- sensitivity to some fabrics.
Allergens
Symptoms of allergic reaction may not appear until several days after exposure. Allergens can include:
- benzocaine
- neomycin
- chlorhexidine (in K-Y Jelly)
- imidazole antifungal
- propylene glycol (a preservative used in many products)
- fragrances
- tea tree oil
- latex (in condoms and diaphragms).
Adapted from The V Book by Elizabeth G. Stewart, M.D., and Paula Spencer (Bantam Books, 2002).
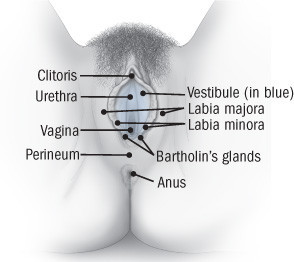
Anatomy of the vulvaThe vulva (Latin for womb or covering) consists of several layers that cover and protect the sexual organs and urinary opening. The fleshy outer lips of the vulva — the labia majora — are covered with pubic hair and contain fat that helps cushion the area. Inside the labia majora are the thinner, more pigmented and delicate flaps of skin called the labia minora. The labia minora join at the top to enclose the clitoris.
The labia majora, labia minora, and clitoris are made up of erectile tissue, that is, tissue that can become engorged with blood. The area between the labia minora, the vestibule, contains the openings to the urethra and the vagina, as well as the Bartholin's glands, which are located on either side of the vaginal opening and produce lubricant for the vestibule. The flesh between the vaginal opening and the anus (not part of the vulva but often involved in vulvar skin problems) is the perineum. This is where the incision called an episiotomy is sometimes made during childbirth, and also where tears can occur on their own during normal childbirth. |
Getting a diagnosis for vulvar skin conditions
Vulvar skin conditions are highly treatable, but the treatment depends on the specific cause. And identifying the underlying diagnosis can be very challenging.
Tell your clinician about any other past or present medical conditions (including bladder and bowel issues) and any skin problems elsewhere on your body.
For example, psoriasis anywhere on the body raises the risk of lichen sclerosus. Crohn's disease, a chronic inflammatory intestinal disease, may cause abscesses or draining fistulas in the vulvar area, and vulvar skin problems are often one of its early symptoms. Lichen planus is another cause of vulvovaginal problems. (The term "lichen," as applied to skin disorders, refers fancifully to skin lesions that resemble lichen on rocks.)
Long-term treatment with oral steroids, immune suppressants, or antibiotics can affect vulvar skin and raise the risk of infection.
Your clinician will want to know how you care for your vulvar skin, which can help identify possible sources of irritation. Even if you can't pinpoint a change, that doesn't mean your standard routine isn't the culprit. Sometimes vulvar problems are the cumulative effect of long-term practices.
It's often what you've done day after day, year after year, that causes the problem. If you wear abrasive clothing and engage in abrasive activities like bicycling or spinning class, and wear tight workout clothes that expose your vulva to sweat or to detergent or soap residue, eventually it might catch up with you.
Report all the symptoms that concern you, including itching, burning, soreness, discoloration, discharge, bumps, and any rashes the vulva. It will also help if you can provide a history of your symptoms and recall what seems to make them better or worse.
Your clinician will examine the vulva, perhaps using a magnifying glass, and insert a speculum to inspect the vagina. She or he may test the pH (acid-base balance) of the vagina, and take samples of secretions to examine under the microscope or culture for yeast. Remember, even if you're seeing an experienced clinician, several visits may be needed to diagnose and improve certain vulvovaginal conditions.
The problem with self-treatment
When vaginal or vulvar itching occurs, women usually assume it's a yeast infection and treat it with an over-the-counter antifungal cream. Often this does the trick, but not always. Instead, the cause of the symptoms might be dry skin, a sexually transmitted disease or bacterial infection, a less common strain of yeast that requires special medication, or irritation by and allergic reactions to common products such as soaps, creams, and lotions.
If yeast isn't the problem, an antifungal cream isn't the solution. And if your skin is already irritated, you may exacerbate the problem by introducing preservatives (such as alcohol or propylene glycol) and other ingredients contained in many antifungal remedies. That's why it's important to see your gynecologist or dermatologist if a problem persists after you've tried a standard antifungal cream.
Another common response of women faced with a vaginal discharge or itch is to wash the vulvar skin vigorously, on the assumption that this will disinfect the area or remove irritants. But aggressive cleansing can add to the irritation, and won't get rid of the underlying problem. Until the problem is diagnosed, it's best to follow a gentle skin care routine (see "Gentle vulvar care").
In fact, gentle cleansing applies whether you have a vulvar skin condition or not: Wash the area gently with your fingertips or a soft cloth and pat dry with a soft towel. Don't use a rough washcloth, and don't rub.
Gentle vulvar careWhether you have a vulvar skin problem or are just prone to irritation, gentle care of the area is a must. The following gentle care tips may help relieve vulvar itching, dryness, and irritation:
|
Some women with vulvar skin problems may benefit from estrogen therapy (delivered vaginally via ring, tablet, or cream, or applied directly to the vulva), which can help counter atrophy and inflammation and make the vulvar skin less vulnerable to irritation.
Image: michaeljung/Getty Images
About the Reviewer

Toni Golen, MD, Editor in Chief, Harvard Women's Health Watch; Editorial Advisory Board Member, Harvard Health Publishing; Contributor
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.