When sex hurts
Pain shouldn’t interfere with pleasure, so don’t leave this problem between the sheets.
- Reviewed by Toni Golen, MD, Editor in Chief, Harvard Women's Health Watch; Editorial Advisory Board Member, Harvard Health Publishing; Contributor, and
- Hope Ricciotti, MD, Editor at Large, Harvard Women's Health Watch

In the movies, amazing sex always seems like an easy home run. But real-life sex can throw us some curve-balls — including pain that interferes with moments we once counted on to bring nothing but pleasure.
Painful sex is a problem many shove under the covers, since it can be awkward to discuss, even with a doctor. But if you’re dealing with it, you’re far from alone. Discomfort during intercourse is exceedingly common, with nearly three-quarters of women experiencing it at some point in their lives, according to the American College of Obstetricians and Gynecologists. And up to six in 10 women report painful sex during the ramp-up to menopause and beyond.
"Strong research shows that women often don’t share this concern with their health care providers unless they’re specifically asked, and doctors rarely ask," says Dr. Jan Shifren, director of the Midlife Women’s Health Center at Harvard-affiliated Massachusetts General Hospital. "I think there’s some embarrassment on both sides."
What characterizes painful sex? It might include not just jabs or twinges of pain itself, but also burning, soreness, dryness, or an overall sense of discomfort. It’s typically most noticeable in the vagina and vulva but can extend to surrounding areas that include the pelvis and lower back. Pain can also occur with solo sexual activity and with partners of any gender.
But you don’t have to settle for sex that hurts. When pleasure turns to pain, it’s time to investigate why — and pinpoint ways to bring fun back into the bedroom. "Physical intimacy is important for couples," Dr. Shifren says. "I’ve had women come to me and say, ‘We both really want penetrative sex back in the relationship.’"
Reasons for pain
Why might sex become painful, especially after years of consistently comfortable lovemaking? The reasons largely depend on your season of life but also encompass other wide-ranging factors. Gynecologic conditions such as fibroids, ovarian cysts, endometriosis, and pelvic inflammatory disease may contribute. So might other health issues, such as cancer, pelvic surgery or radiation, or arthritis. Vulvodynia, a chronic pain disorder affecting the vulva, can make even the idea of sex unthinkable.
But the following scenarios explain most cases of painful sex, Dr. Shifren says.
Childbirth. Delivering a baby vaginally is unquestionably hard on the vagina — sometimes more so for women who had an episiotomy or tears in the perineum. "It can take several months to heal," she says. Hormone fluctuations after childbirth and while breastfeeding can also lead to vaginal dryness, compounding the issue.
Menopause. Decreasing estrogen levels during the years leading to menopause and beyond can trigger a creeping, chronic lack of natural vaginal lubrication. "It typically starts with a sense of dryness or soreness low in the vagina, but over time it can become really uncomfortable everywhere," she says.
Hypertonic pelvic floor. This automatic tightening of the muscles surrounding the vaginal opening can occur after a traumatic event, such as a sexual assault. But even the thought of pain in the bedroom can, ironically, lead to the condition. This becomes a vicious cycle; the more you anticipate that sex will be painful, the more the pelvic floor muscles contract. "It’s almost like your body is trying to protect you, and your pelvic floor muscles tighten up when-ever intercourse is attempted, making sex even more painful," she says. "It can feel like there’s a wall there."
Ways to improve comfort
Sex can lose its luster if you’re worried it will hurt. But the adage to "use it or lose it" doesn’t apply here: having less sex as menopause approaches doesn’t make painful intercourse more likely, according to a new analysis.
The study, published June 1, 2022, in Obstetrics and Gynecology, involved 2,247 women ages 42 through 52 who reported no sexual pain at the study’s start and agreed to log sexual frequency and symptoms. During up to 10 follow-up visits over the following 13 years, nearly half reported developing pain during sex at least sometimes. Vaginal dryness showed the strongest link, while having oral sex or being aroused more often (with or without sexual activity) were linked to lower odds of sexual pain. But the amount of sex women had didn’t factor in.
"We used to think that intercourse is good for the vagina, stretching it and bringing in secretions and blood flow," Dr. Shifren says. "But there are no data that support this. I would never tell a patient who’s having painful sex that the treatment is to have sex."
If painful sex is frequent or severe, however, Dr. Shifren advises a gynecologic visit, which should include a thorough history and a pelvic exam. An ultrasound may be performed if you’re experiencing sexual pain deep within the pelvis. But the exam, along with your descriptions, will largely guide the diagnosis and the choice of treatment. The following are among the most common options:
Lubricants. These can lessen friction, irritation, and sensitivity when the vagina is penetrated. Many are available over the counter, including water-soluble products as well as silicone-based versions that last longer and are typically more slippery. Even cooking oils such as olive or coconut can do double duty in the bedroom. Whatever you choose, make sure it’s hypoallergenic, with no added colors or flavors that can irritate tissues. But if you’re also using condoms, avoid petroleum jelly, baby oil, or mineral oil, which can lead to breaks.
Vaginal moisturizers. These products differ from lubricants by prompting cells in the vagina to pull in water instead of simply making the passage more slippery. "It’s like moisturizing your hands or your face," Dr. Shifren says. Most are long-acting, designed to be used several days a week.
Vaginal estrogen. Coating the inside of the vagina with a prescription estrogen product can restore plumpness to thinning tissues, boosting both moisture and comfort during intercourse. It’s available in several forms, including creams and suppositories that are used a few times a week. A longer-acting option is a soft, flexible estrogen ring (Estring) that continuously releases tiny amounts of the hormone over three months. Prescription estrogens can be expensive, Dr. Shifren says, but are considered extremely safe. They don’t raise blood estrogen levels, skirting potential health risks of higher-dose, systemic hormone therapy used to treat hot flashes and other menopause symptoms.
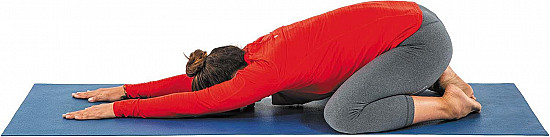
Pelvic floor physical therapy. Many therapists are trained to focus on only the pelvic floor, stretching or strengthening tissues as needed and teaching women exercises to relax the pelvic floor muscles. "It can be life-changing for women experiencing pelvic pain and painful sex that doesn’t respond to other treatments," Dr. Shifren says.
When it comes to sexual comfort, sometimes the best thing to stretch is your mind. Consider alternate ways of giving and receiving pleasure, Dr. Shifren says. "Sex should be broadly defined and can be pleasurable without penetration," she says. "Many women and couples engage in sex involving the external genitals or oral activities, becoming more creative as years pass."
Image: © valentinrussanov/Getty Images
About the Author

Maureen Salamon, Executive Editor, Harvard Women's Health Watch
About the Reviewers

Toni Golen, MD, Editor in Chief, Harvard Women's Health Watch; Editorial Advisory Board Member, Harvard Health Publishing; Contributor

Hope Ricciotti, MD, Editor at Large, Harvard Women's Health Watch
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.